Hypertension Drugs: What They Are and Why They Matter
When talking about Hypertension Drugs, medications prescribed to lower elevated blood pressure and prevent heart‑related complications. Also known as high‑blood‑pressure meds, they are a key part of modern cardiovascular care. Hypertension drugs come in several families, each with its own way of calming the circulatory system. The most common groups are ACE Inhibitors, agents that block a hormone that narrows blood vessels, Beta Blockers, drugs that slow the heart’s rhythm and reduce force of contraction, and Calcium Channel Blockers, medicines that relax the muscle cells of arteries. Together, these drug families help keep systolic and diastolic numbers in a healthier range, which in turn cuts the odds of stroke, kidney damage, and heart attack. Understanding which class you’re on, why it was chosen, and how it fits into the bigger picture of blood‑pressure control makes it easier to stick with treatment and notice when something feels off.
How Hypertension Drugs Connect with Other Health Issues
High blood pressure doesn’t exist in a vacuum; it often links to blood‑clot risk, heart‑failure signs, and the need for anticoagulants like warfarin. When you take a drug that lowers pressure, the strain on vessel walls eases, which can lower the chance of clots forming in places like stents. That’s why doctors sometimes pair a blood thinner, such as warfarin, to protect against clotting while managing blood pressure. The interaction between hypertension drugs and blood thinners is a classic example of how medication classes influence each other—your heart health team will usually monitor INR levels closely if you’re on both.
Lifestyle changes act as a partner to medication. Regular exercise, reduced salt intake, and stress‑cutting habits can boost the effect of any hypertension drug you’re using. Think of it as a two‑handed approach: the drug works chemically, while diet and activity give the cardiovascular system a chance to stay steady without relying solely on chemicals. Many patients report that after a few weeks of pairing a low‑dose ACE inhibitor with modest treadmill walks, their daily blood‑pressure readings drop more than the pill alone would achieve.
What should you keep an eye on when you start a hypertension drug? Common side effects differ by class—dry cough is typical for ACE inhibitors, fatigue can pop up with beta blockers, and swollen ankles sometimes appear with calcium channel blockers. Your doctor will likely schedule follow‑up visits, check blood‑pressure logs, and maybe run basic blood tests to make sure electrolytes stay balanced. Knowing the typical signs early helps you talk to your provider before a problem becomes serious.
Below you’ll see a collection of articles that dive deeper into specific drug types, safety tips, and how hypertension meds intersect with topics like clot formation, heart‑stent care, and lifestyle adjustments. Whether you’re new to treatment or looking for a refresher, the posts ahead give practical advice you can apply right away.
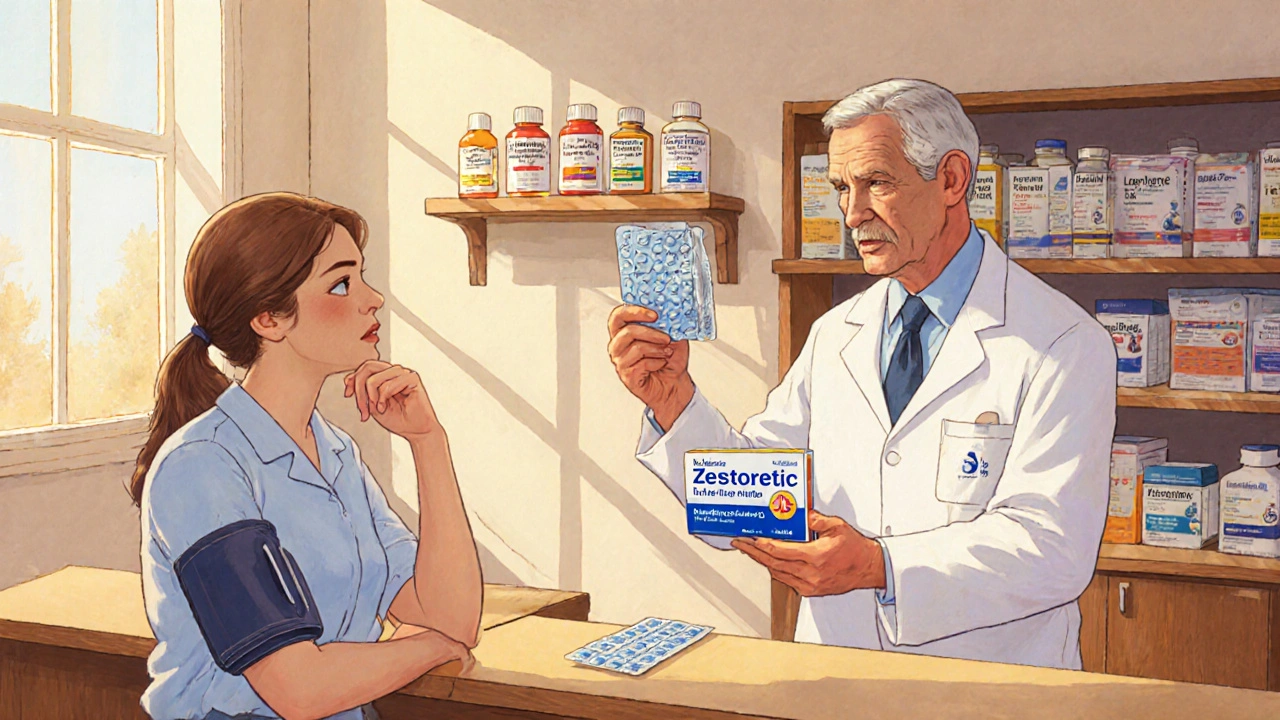
Zestoretic vs Alternatives: Which Hypertension Combo Works Best?
A detailed comparison of Zestoretic (lisinopril+hydrochlorothiazide) with leading hypertension alternatives, covering efficacy, side‑effects, cost and patient suitability.
view more