Reperfusion Injury: Understanding the Damage When Blood Flow Returns
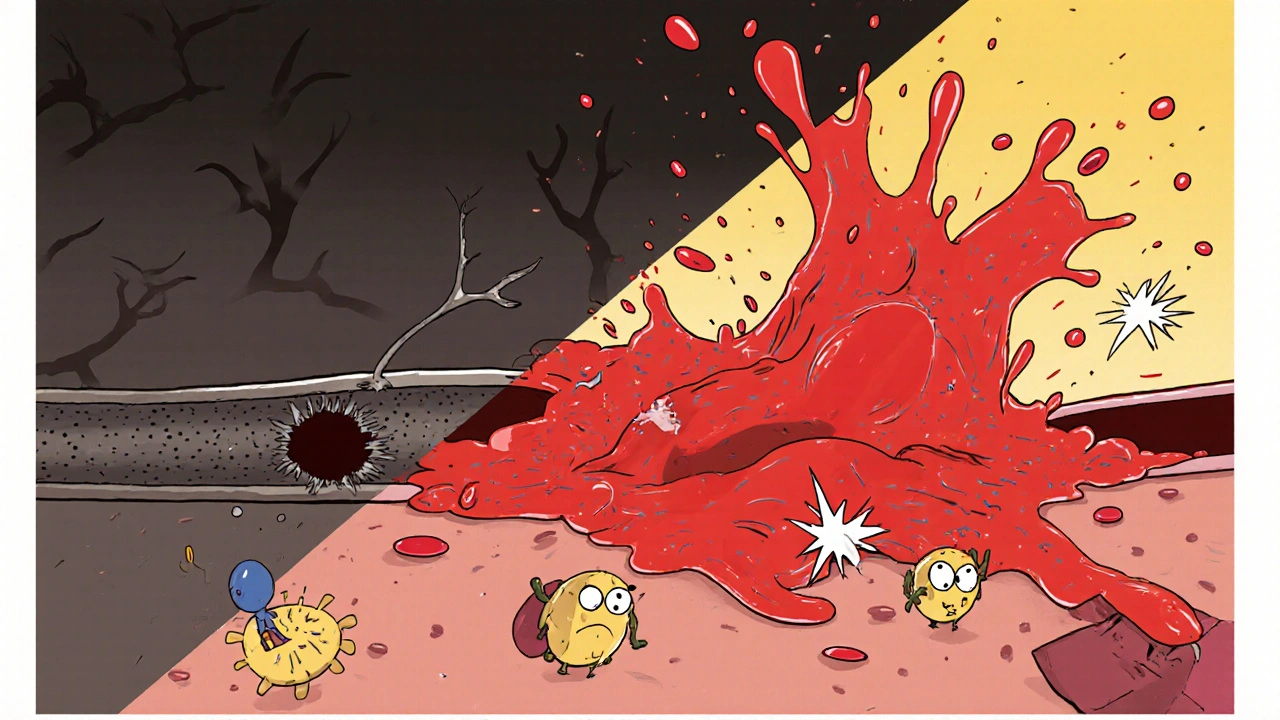
When working with Reperfusion Injury, the tissue damage that follows the restoration of blood flow after a period of blockage. Also known as ischemia‑reperfusion injury, it is a central issue in heart attacks, strokes, and organ transplants. The problem starts with Ischemia, a state where cells are starved of oxygen and nutrients. Once the blockage is cleared, the sudden rush of oxygen triggers a burst of harmful chemistry, turning a rescued organ into a new source of injury. In plain terms, reperfusion injury is the price we pay for getting blood back to starving tissue, and it shows up as swelling, cell death, and loss of function.
Key Factors Behind Reperfusion Injury
The cascade that follows blood return is driven by Oxidative Stress. When oxygen floods the cells, it reacts with vulnerable molecules to create free radicals—highly reactive particles that shred membranes, proteins, and DNA. At the same time, Inflammation ramps up as immune cells rush in, releasing cytokines that worsen the damage. These three elements—ischemia, oxidative stress, and inflammation—form a loop where each amplifies the others. The result is calcium overload inside cells, mitochondrial dysfunction, and ultimately, irreversible cell death. Researchers have shown that limiting any one of these steps can cut the overall injury by a significant margin, which is why therapeutic strategies often target multiple points in the pathway.
Clinically, reperfusion injury matters because it can undo much of the benefit we gain from procedures that open blocked arteries or restore organ perfusion. Doctors use drugs that act as antioxidants, such as N‑acetylcysteine, or agents that block specific inflammatory signals to blunt the harmful surge. Pre‑conditioning—briefly exposing tissue to short periods of ischemia before a major blockage—trains the cells to handle the oxidative hit more gracefully. Emerging therapies like mitochondria‑targeted peptides and gene‑editing approaches aim to break the cycle at its source. Understanding how the three core entities interact helps clinicians choose the right mix of interventions for each patient. Below, you’ll find a curated set of articles that dive deeper into the science, real‑world case studies, and practical tips for managing reperfusion injury across different medical contexts.
Reperfusion Injury and Immune System Disorders: In‑Depth Overview
Explore how reperfusion injury intertwines with immune disorders, its key players, clinical impact, and the latest therapeutic strategies.
view more