Blood Clot: Causes, Risks, and Treatment Options
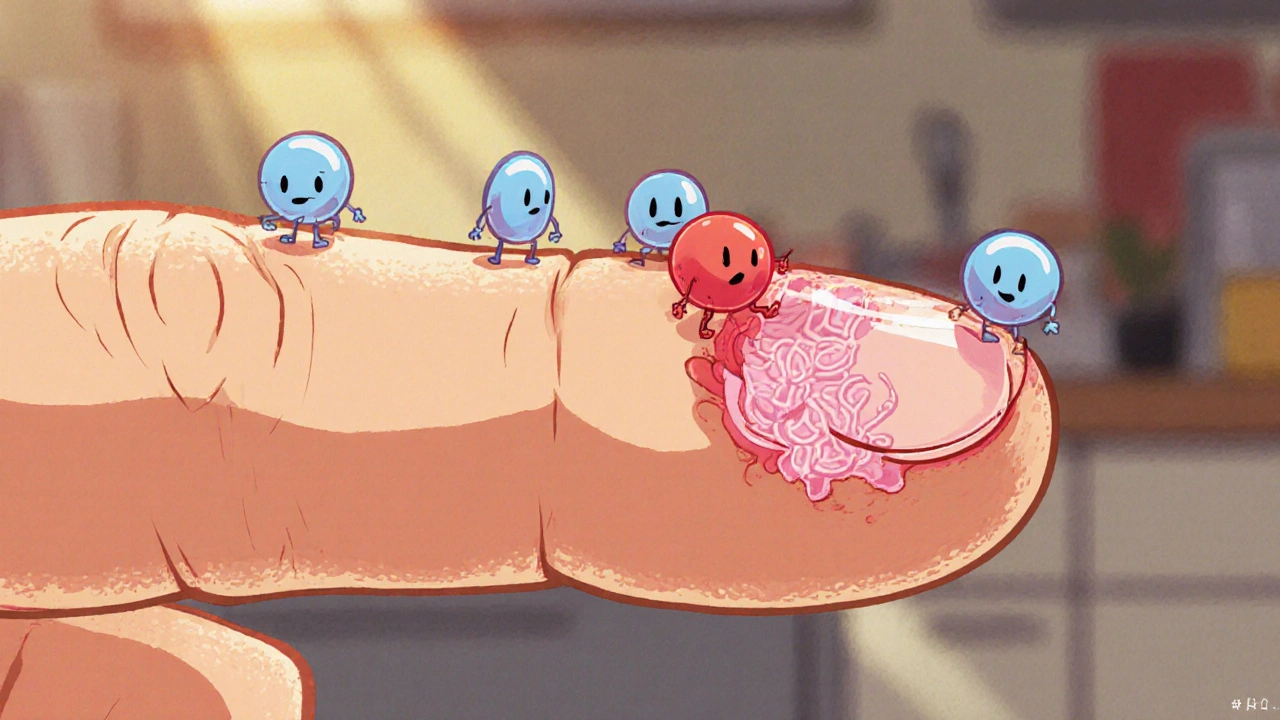
When you hear the term blood clot, a solid mass of blood cells, platelets, and fibrin that forms inside a vessel or the heart. It’s also called a thrombus, and it can block circulation, lead to tissue damage, or even be life‑threatening.
One of the most common ways a clot shows up is as deep vein thrombosis, a condition where a clot builds up in the deep veins of the leg. Blood clot formation often follows three steps: platelets stick together, fibrin weaves a mesh, and the clot stabilizes. Risk factors include long periods of immobility, recent surgery, certain cancers, hormonal therapy, and inherited clotting disorders. Typical signs are swelling, warmth, and pain in the calf or thigh; if you notice these, a prompt ultrasound can confirm the diagnosis. Detecting a clot early can mean the difference between a simple anticoagulant prescription and a serious emergency.
How Treatment and Related Issues Interact
To break or prevent a clot, physicians prescribe anticoagulant therapy, drugs like warfarin, apixaban, or heparin that thin the blood and stop the clot from growing. In urgent cases, clot‑busting medication called thrombolytics may be used, but they carry a bleeding risk. Patients on anticoagulants need regular blood‑test monitoring—usually the INR for warfarin—to keep the dose in the safe range. Diet matters too; vitamin K‑rich foods can interfere with warfarin, so a consistent eating pattern helps maintain stable blood levels.
Another scenario where clots cause trouble is stent thrombosis, where a clot forms inside a coronary stent placed to keep an artery open. This type of clot can trigger chest pain, heart attack, and even affect sexual health by reducing blood flow to the pelvic region. Managing stent thrombosis usually means a combination of dual antiplatelet therapy, lifestyle changes such as quitting smoking, controlling cholesterol, and regular follow‑up imaging.
Recent research links reperfusion injury—a burst of oxygen when blood flow returns after a blockage—to new clot formation. The sudden oxidative stress can activate platelets, creating a fresh thrombus that complicates recovery. Understanding this connection helps clinicians decide when to give additional antithrombotic drugs after procedures like angioplasty.
Beyond the heart, clotting can disrupt other systems. For example, urinary retention sometimes follows bladder muscle spasms that are worsened by clot‑related inflammation. Infections, skin breakdown, or even severe acid reflux can indirectly raise clot risk by promoting systemic inflammation. Simple steps—staying hydrated, wearing compression stockings after surgery, and doing regular leg‑raising exercises—can lower the chance of a clot forming in the first place.
Pregnant women and people on hormone‑based birth control also face a higher clot risk because estrogen can increase clotting factors. In these cases, doctors may monitor more closely or suggest alternative contraception. If you’re dealing with hypertension, the medication combo Zestoretic (lisinopril + hydrochlorothiazide) can influence fluid balance, which indirectly affects clotting tendencies—another reason why a full medication review is essential.
Below you’ll find a curated list of articles that dig deeper into each of these topics—whether you’re looking for a side‑by‑side drug comparison, an explanation of how clots affect stents, or lifestyle tips to keep your blood flowing smoothly. Dive in to get the details you need to make informed health decisions.
How Blood Clots Form and Dissolve: The Science Explained
Explore how blood clots form, the chemistry behind clot dissolution, and what happens when the process goes wrong, with clear tips to stay healthy.
view more