Clot Risk Assessment Tool
Blood Clot Risk Assessment
Answer questions to assess your risk of abnormal clot formation based on the science explained in the article.
Risk Assessment Results
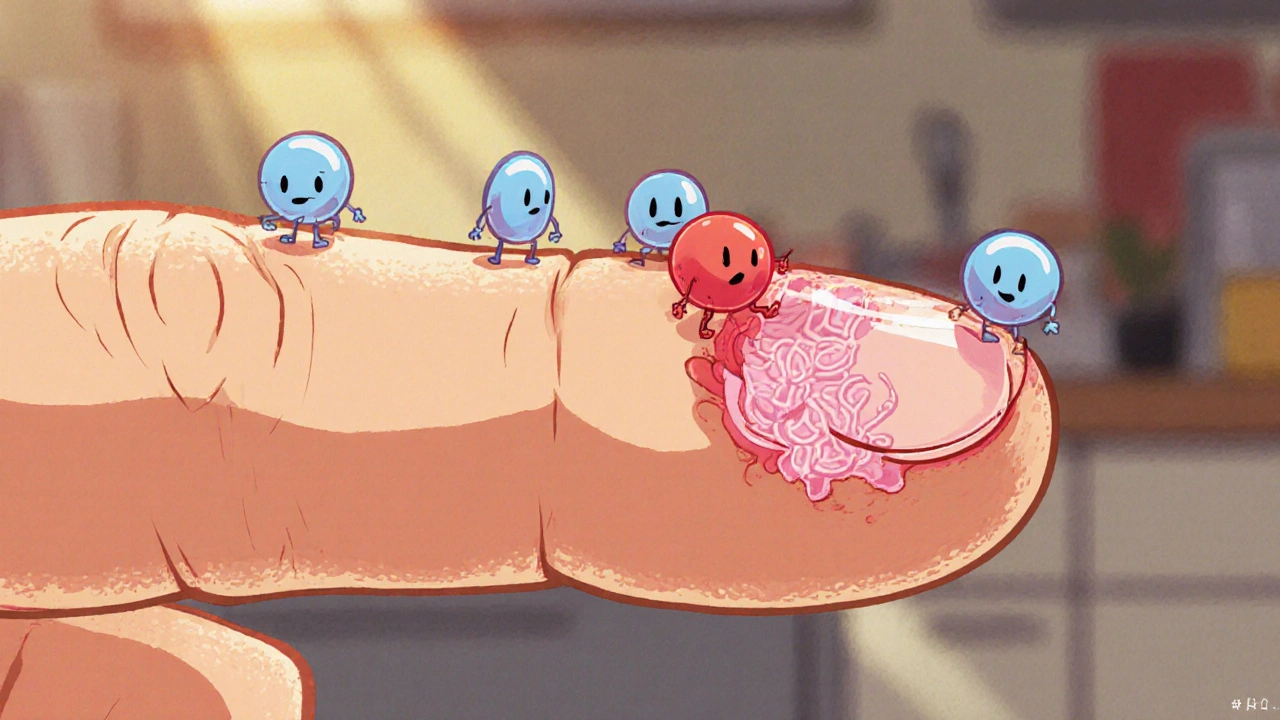
Ever wonder why a tiny cut on your finger stops bleeding in seconds? That rapid fix is a well‑orchestrated series of events called hemostasis, and at its heart lies the blood clot. Understanding how our bodies create and later break down these clots can demystify everything from a simple scrape to life‑threatening strokes.
Platelet Plug: The First Line of Defense
When a blood vessel is injured, the inner lining (the endothelium) ruptures, exposing collagen fibers beneath. This is the cue that platelet a tiny, disc‑shaped cell fragment that circulates in the blood can’t ignore. Within seconds, platelets change shape, become sticky, and cling to the exposed collagen, forming a loose “platelet plug.”
Platelets also release chemical messengers like ADP and thromboxane A2, which recruit more platelets to the site. Think of it as a rapid construction crew shouting, “More hands, please!” This plug is fragile, but it buys time for the next, stronger phase.
The Coagulation Cascade: Building a Fibrous Mesh
While the platelet plug is forming, a cascade of plasma proteins-known as clotting factors-activates in a domino effect. Each step converts an inactive protein (a zymogen) into an active enzyme. The cascade splits into two pathways: the intrinsic (contact) pathway and the extrinsic (tissue factor) pathway, both converging on a pivotal player, thrombin an enzyme that converts fibrinogen into fibrin.
Thrombin’s job is to turn soluble fibrinogen, a protein floating in plasma, into insoluble fibrin strands. These strands weave through the platelet plug, creating a sturdy net that traps red blood cells and seals the wound. The end product-a stable blood clot a mesh of fibrin and platelets that blocks bleeding-is now firm enough to withstand blood pressure.
Key Factors that Influence Clot Formation
- Vitamin K a fat‑soluble vitamin essential for activating several clotting factors. Deficiency slows clotting, while excess can tip the balance toward hyper‑coagulation.
- Heparin an anticoagulant that enhances antithrombin III, slowing thrombin formation. Used medically to prevent unwanted clots during surgery.
- Genetic mutations such as Factor V Leiden make clotting factors more resistant to natural inhibitors, raising thrombosis risk.
- Inflammation and endothelial damage from smoking or high blood pressure accelerate the cascade.
Balancing these elements is crucial-too little clotting leads to hemorrhage, too much leads to dangerous blockages.
How Clots Dissolve: The Fibrinolytic System
Once the vessel heals, the body must remove the clot. This cleanup crew is called fibrinolysis the process that breaks down fibrin using the enzyme plasmin. The liver secretes plasminogen, an inactive precursor that binds to fibrin fibers. Tissue plasminogen activator (tPA), released from intact endothelial cells, converts plasminogen into active plasmin.
Plasmin then slices fibrin strands into soluble fragments, which the bloodstream carries away. In a healthy adult, this cycle of clot formation and dissolution repeats countless times without us noticing.
| Aspect | Clot Formation (Hemostasis) | Clot Dissolution (Fibrinolysis) |
|---|---|---|
| Primary Actors | Platelet, Thrombin, Fibrin | Plasmin, tPA, Plasminogen |
| Trigger | Vessel injury exposing collagen | Endothelial recovery, tPA release |
| Goal | Seal breach, prevent blood loss | Remove the seal once repair is complete |
| Regulation | Vitamin K‑dependent factors, antithrombin III | α2‑antiplasmin, plasminogen activator inhibitor‑1 (PAI‑1) |
When the System Falters: Thrombosis, DVT, and Pulmonary Embolism
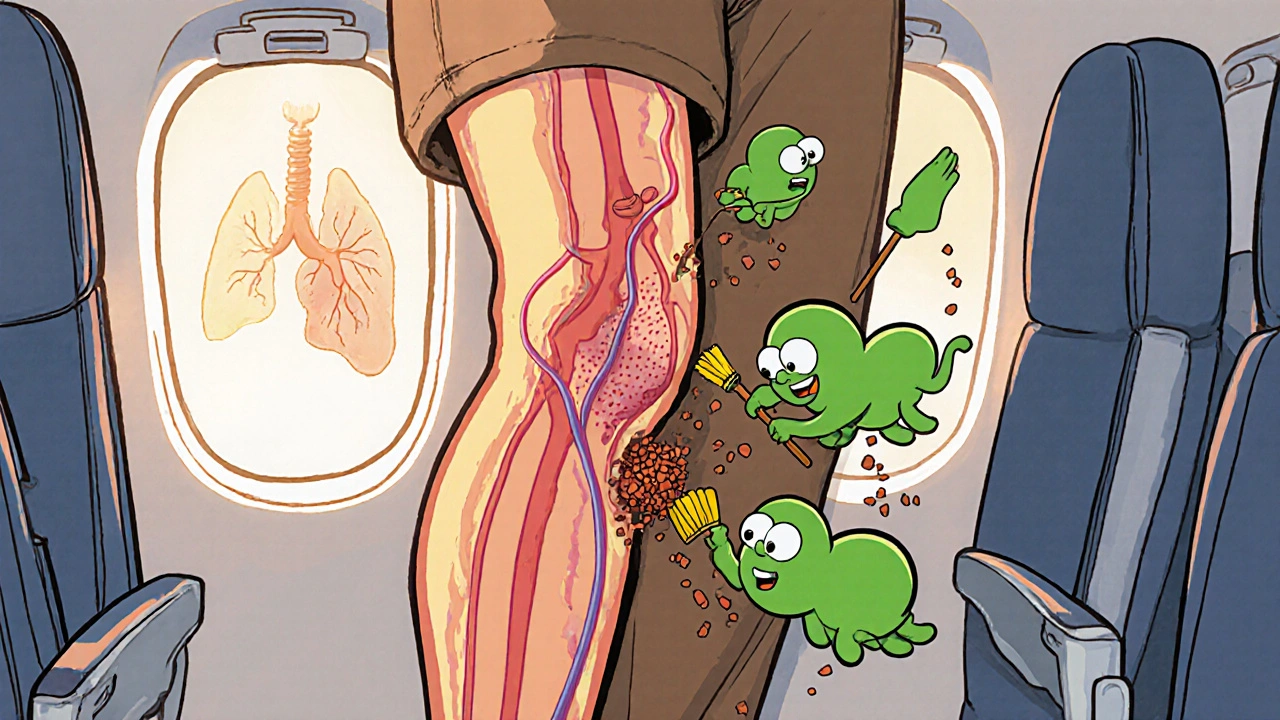
If clotting goes overboard, the result is a thrombosis-an unwanted clot forming inside a vessel. Deep vein thrombosis (DVT) commonly occurs in the legs’ vena cava the large vein returning blood to the heart or its branches. A piece of a DVT clot can break off, travel through the heart, and lodge in the lungs, causing a pulmonary embolism (PE), a medical emergency.
Risk factors include prolonged immobility (long flights), cancer, pregnancy, and inherited clotting disorders. Symptoms may be swelling, pain, or sudden shortness of breath. Prompt diagnosis via ultrasound or D‑dimer testing can save lives.
Keeping the Balance: Lifestyle and Medical Strategies
Maintaining a healthy clotting system is part science, part habit. Here are practical steps:
- Stay active: Walking every hour during long trips keeps blood flowing.
- Eat vitamin‑K‑rich foods like kale, broccoli, and spinach-but keep intake consistent if you’re on anticoagulants.
- Limit smoking and excessive alcohol, both of which damage the endothelium.
- Follow prescribed anticoagulants (e.g., Heparin a fast‑acting blood thinner used in hospitals or newer oral agents) exactly as directed.
- Know your family history: Inherited conditions like Factor V Leiden may require screening.
By integrating these habits, you support the body’s natural equilibrium between clotting and clot breakdown.
Quick Checklist: What to Remember About Blood Clots
- Platelets start the plug; thrombin creates fibrin.
- Vitamin K activates clotting factors; heparin blocks them.
- Fibrinolysis, driven by plasmin, dissolves the clot after healing.
- Uncontrolled clotting leads to DVT, PE, and strokes.
- Movement, balanced diet, and medication adherence keep the system in check.
Frequently Asked Questions
What triggers the clotting cascade?
A breach in the blood vessel wall exposes collagen and tissue factor, which activate the intrinsic and extrinsic pathways of the cascade, eventually producing thrombin.
How does the body prevent clots from growing too big?
Natural inhibitors like antithrombin III, protein C, and α2‑antiplasmin keep clotting factors and plasmin in check, ensuring clots stay localized.
Can diet affect clotting risk?
Yes. Vitamin K‑rich foods boost clotting factor activation, while excessive saturated fats and trans fats can increase inflammation and clot propensity.
What are the warning signs of a dangerous clot?
Sudden leg swelling, pain, warmth, or redness may indicate DVT. Shortness of breath, chest pain, or rapid heartbeat could signal a pulmonary embolism.
Is fibrinolysis the same as taking clot‑busting drugs?
The body’s fibrinolysis uses tPA and plasmin naturally. Medical clot‑busting drugs (e.g., recombinant tPA) boost this process during strokes or heart attacks.
Bethany Torkelson
October 18, 2025 AT 18:46Wow, reading about how our bodies instantly seal a cut is mind-blowing. The way platelets rush in like tiny emergency workers is something I never appreciated. It's crazy how this invisible process saves us every single day. I feel a surge of gratitude for every little clot that never lets me bleed out.
Margaret pope
October 19, 2025 AT 20:53Great breakdown of the clotting steps lets people really see the flow of the cascade without getting lost in jargon
Karla Johnson
October 19, 2025 AT 22:16The cascade you described is a remarkable example of biochemical engineering operating at breakneck speed. When a vessel is breached, the endothelial lining no longer shields collagen, exposing a molecular alarm signal that instantly recruits platelets to the site. Those platelets undergo a rapid shape change, extending pseudopods and becoming sticky, which allows them to adhere firmly and form a provisional plug. Simultaneously, they release ADP and thromboxane A2, amplifying the recruitment signal and ensuring that the plug expands quickly enough to stem the bleed. Meanwhile, the extrinsic pathway kicks in as tissue factor binds to factor VII, forming a complex that activates factor X. In parallel, the intrinsic pathway is triggered when exposed collagen activates factor XII, setting off a chain reaction that also converges on factor X. Activated factor X, together with its cofactor Va, converts prothrombin to thrombin, a pivotal enzyme that not only transforms fibrinogen into insoluble fibrin strands but also reinforces platelet activation through feedback loops. Fibrin polymerizes into a mesh that traps red blood cells, solidifying the clot into a stable structure capable of withstanding arterial pressure. Vitamin K is essential here because it enables gamma‑carboxylation of several clotting factors, without which the cascade would stall. Conversely, anticoagulants like heparin boost antithrombin III activity, dampening thrombin formation and preventing excessive clotting. Once the vessel wall repairs, endothelial cells release tissue‑type plasminogen activator (tPA), which converts plasminogen bound to fibrin into plasmin, the enzyme that degrades the fibrin mesh. This fibrinolytic process restores normal blood flow and clears the debris of the healed wound. Dysregulation at any point-whether hyperactive platelets, over‑production of thrombin, or insufficient plasmin activity-can tip the balance toward pathological thrombosis, leading to conditions such as deep‑vein thrombosis or pulmonary embolism. Lifestyle factors like prolonged immobility, smoking, and poor diet can exacerbate these risks by promoting endothelial dysfunction and inflammation. Understanding each step of this cascade not only satisfies scientific curiosity but also guides therapeutic strategies, from vitamin K antagonists to direct oral anticoagulants and clot‑busting agents used in acute stroke. In essence, the clotting and clot‑dissolution system is a finely tuned orchestra, where timing, concentration, and feedback are all crucial for maintaining vascular health.
Linda A
October 21, 2025 AT 00:40One might liken the clotting cascade to a brief, intense dialogue between cells and proteins, a silent negotiation that ends before we even realize it. It is as if the body whispers, and the blood listens, forging a temporary bridge over a breach. When the conversation ceases, the bridge is carefully dismantled, restoring the river’s flow.
Joe Moore
October 21, 2025 AT 01:30Yo, dont you think they hide the real reason behind all these clotting meds? The pharma guys want us on meds forever they hide natural ways like diet and movement they push tpa as miracle drug but its just a way to keep us dependent the system is rigged and we dont even see it coming
Ayla Stewart
October 22, 2025 AT 04:26I appreciate the clear steps you laid out for how clots form and then dissolve. It helps me understand why staying active and eating balanced meals matter for my blood health.
Poornima Ganesan
October 22, 2025 AT 05:50Honestly, most people overlook how easy it is to control clot risk by simply adjusting their diet. If you keep your vitamin K intake consistent, you avoid the wild swings that can mess with anticoagulant dosing. Also, smoking isn’t just a habit; it’s a direct assault on the endothelial lining, making clots more likely. I’ve seen countless cases where a simple lifestyle tweak prevented a DVT, yet people stubbornly ignore the data. Remember, the body prefers balance-over‑supplementation can be as harmful as deficiency. So, stop making excuses and start tracking your intake; you’ll thank yourself later.
Emma Williams
December 19, 2025 AT 17:33Great summary!