Clot Formation: Understanding the Process and Its Health Impact
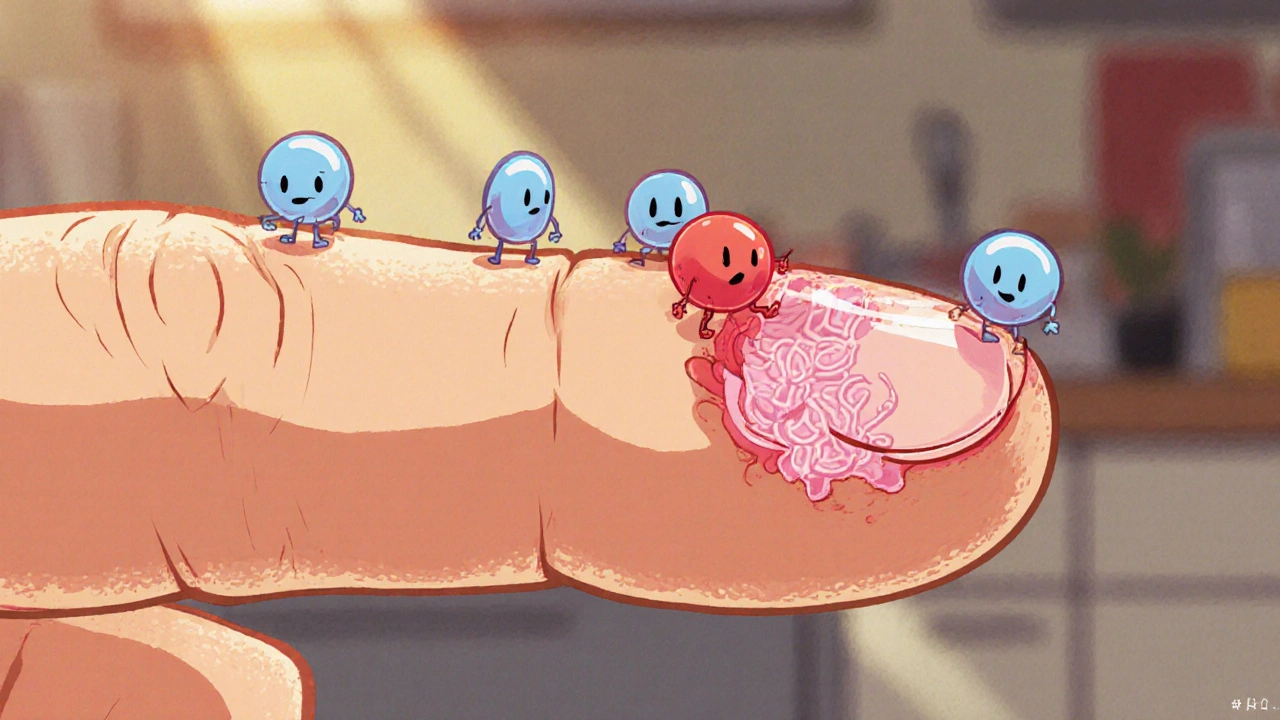
When dealing with clot formation, the body's natural response that turns liquid blood into a solid plug to stop bleeding. Also known as thrombosis, it can protect you or cause serious problems depending on where and how it occurs. A clot starts when blood vessels are injured or when the blood’s chemistry shifts. The first responders are platelets, tiny cell fragments that stick together and form a temporary seal. Soon after, a protein called fibrin weaves a mesh that makes the plug sturdy. In most cases this process saves lives, but when it happens inside a healthy vessel, it blocks blood flow and can lead to heart attacks, strokes, or limb loss.
Understanding Thrombosis, the medical term for an unwanted clot that forms inside a blood vessel. Thrombosis is essentially clot formation gone awry. It can appear in veins (deep‑vein thrombosis) or arteries (arterial thrombosis). The risk rises with factors like high blood pressure, sedentary lifestyle, or certain medications. When a clot lodges in a vein, it may break free and travel to the lungs, causing a pulmonary embolism. In arteries, a blockage can starve heart muscle or brain tissue of oxygen, leading to a heart attack or stroke. Recognizing the difference helps doctors choose the right treatment route.
Platelet aggregation is the engine behind clot formation. When a vessel wall is damaged, platelets change shape, release chemicals, and link together through surface receptors. This creates a plug that quickly seals small cuts. At the same time, the coagulation cascade activates clotting factors, culminating in fibrin production. The balance between platelet stickiness and the body’s natural anticoagulants determines whether a clot stays where it’s needed or spreads to where it shouldn’t. Disruption in this balance—whether from genetics or drugs—can tip the scale toward dangerous clotting.
One of the main ways doctors manage risky clot formation is through anticoagulant therapy, medications that slow down the clotting process by inhibiting specific clotting factors. Common choices include warfarin, direct oral anticoagulants like apixaban, and injectable heparin. These drugs don’t dissolve an existing clot but prevent new ones from forming and give the body a chance to break down the old one naturally. Monitoring is crucial because too much anticoagulation can cause bleeding, while too little leaves the patient vulnerable to thrombosis. Lifestyle tweaks—like staying active, managing weight, and controlling blood pressure—work hand‑in‑hand with medication for best results.
When a clot forms inside a cardiovascular stent, it’s called stent thrombosis, a serious complication where a blood clot blocks a previously placed stent. Stent thrombosis can happen days, weeks, or even months after the procedure and often presents as a sudden chest pain or shortness of breath. Preventing it relies heavily on dual antiplatelet therapy—usually aspirin combined with a P2Y12 inhibitor like clopidogrel. Patients with hypertension, diabetes, or who stop their meds early are at higher risk. Understanding how stent thrombosis fits into the broader picture of clot formation helps cardiologists tailor follow‑up care and adjust drug regimens promptly.
Key Topics Covered
Across the articles below you’ll see how clot formation links to conditions such as hypertension (like the Zestoretic comparison article), reperfusion injury after heart attacks, and even urinary retention where bladder muscle spasms can affect blood flow. Some posts explore how lifestyle choices, medication alternatives, and emerging therapies influence clot risk. Whether you’re a patient looking for practical steps or a health professional needing a quick refresher, the collection gives concrete examples, treatment comparisons, and safety tips that directly relate to the entities we just discussed.
Now that you have a solid grasp of what clot formation is, why it matters, and how it connects to thrombosis, anticoagulation, and stent complications, dive into the specific guides below. You’ll find detailed reviews of drugs, insight into related health issues, and actionable advice to help you manage or prevent dangerous clots.
How Blood Clots Form and Dissolve: The Science Explained
Explore how blood clots form, the chemistry behind clot dissolution, and what happens when the process goes wrong, with clear tips to stay healthy.
view more