Anticoagulant Emergency: What to Do When Blood Thinners Go Wrong
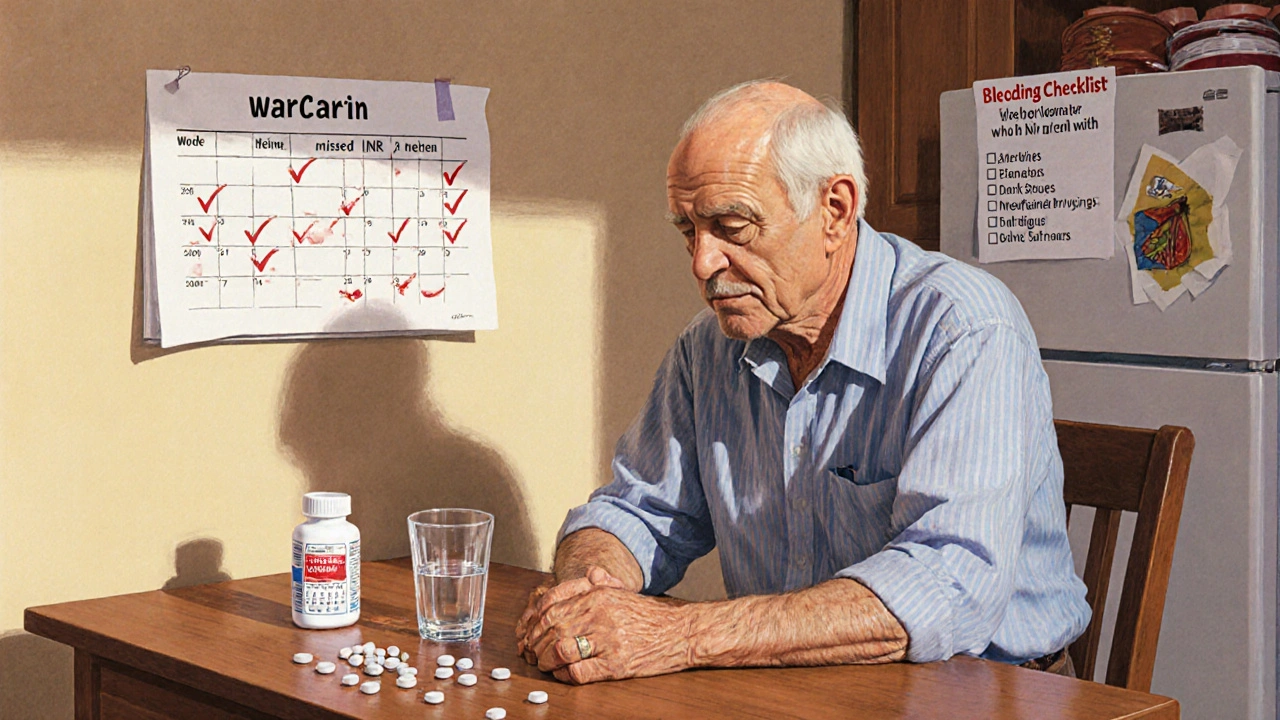
When a person takes a blood thinner—like warfarin, rivaroxaban, or apixaban—and starts bleeding uncontrollably, it’s not just a side effect, it’s an anticoagulant emergency, a life-threatening situation where the body can’t form clots to stop bleeding. Also known as anticoagulant overdose, this isn’t rare. Thousands end up in emergency rooms every year because they didn’t recognize the warning signs until it was too late.
These drugs are meant to prevent clots in people with atrial fibrillation, deep vein thrombosis, or after joint replacements. But if the dose is too high, or if another medication interferes—like antibiotics or NSAIDs—the balance breaks. That’s when you get uncontrolled bleeding, internal or external bleeding that doesn’t stop on its own. It can show up as bruising without injury, blood in urine or stool, vomiting blood, or a sudden, severe headache from brain bleeding. And if someone is on a direct oral anticoagulant (DOAC), there’s no quick lab test to check levels like there is with warfarin. That’s why timing and symptoms matter more than numbers.
Not all anticoagulant emergencies are the same. Some need immediate reversal. For warfarin, doctors use vitamin K and fresh frozen plasma. For newer drugs like Eliquis or Xarelto, there are specific reversal agents, drugs designed to block the anticoagulant effect within minutes. Also known as antidotes for blood thinners, agents like andexanet alfa and idarucizumab can turn the tide—but only if given fast. Delay by even an hour can mean the difference between recovery and permanent damage. Meanwhile, patients on these meds need to know what to avoid: alcohol, herbal supplements like ginkgo or garlic, and even some OTC painkillers. Many don’t realize that a simple fall or cut can turn deadly if they’re on the wrong dose.
What you’ll find in the posts below isn’t theory—it’s real-world guidance from people who’ve been there. You’ll see how drug interactions with antibiotics or supplements can push someone into crisis. You’ll learn why telling your doctor about every pill you take isn’t optional—it’s survival. And you’ll find clear advice on what to do if you or someone you love starts showing signs of internal bleeding. No fluff. No jargon. Just what you need to act fast, stay informed, and keep your anticoagulant therapy safe.
Blood Thinner Overdose and Internal Bleeding: What to Do Immediately
Blood thinner overdose can cause silent, life-threatening internal bleeding. Learn the warning signs, what to do immediately, how doctors treat it, and how to prevent it from happening.
view more