Taking a blood thinner like warfarin, Eliquis, Xarelto, or Pradaxa can save your life by preventing deadly clots. But if you take too much - even by accident - it can cause internal bleeding that kills in hours if not treated fast. This isn’t theoretical. Every year, over 33,000 Americans end up in the emergency room because of blood thinner mistakes. Many don’t realize they’re in danger until it’s too late.
How Blood Thinners Work - and Why Overdose Is So Dangerous
Blood thinners don’t actually thin your blood. They slow down your body’s ability to form clots. Warfarin blocks vitamin K, which your liver needs to make clotting factors. Newer drugs like apixaban and rivaroxaban block specific proteins (Factor Xa) that trigger clotting. These are powerful tools - but they leave you vulnerable to bleeding.
Overdose doesn’t mean you took 10 pills at once. It can happen slowly. A small extra dose every day for a week can build up. Your INR (a blood test that measures clotting time) might creep from 2.5 to 8.0 without you noticing. At INR above 4.5, your risk of serious bleeding jumps sharply. At INR over 10, your body can’t stop bleeding from even a tiny cut.
Signs of Internal Bleeding You Can’t Ignore
Internal bleeding doesn’t always look like a gushing wound. It’s often silent until it’s critical. Here’s what to watch for:
- Black, tarry, or bloody stools - this means bleeding in your stomach or intestines
- Pink, red, or dark brown urine - blood in your kidneys or bladder
- Coughing or vomiting blood, or material that looks like coffee grounds
- Unexplained bruising - especially large, spreading bruises with no injury
- Small red or purple dots under the skin (petechiae) - tiny broken blood vessels
- Heavy or prolonged menstrual bleeding - more than soaking a pad every hour
- Severe headache, dizziness, confusion - could mean bleeding in the brain
- Sharp pain in your abdomen, back, or chest - possible internal organ bleeding
- Extreme fatigue or shortness of breath - signs your body is losing too much blood
One patient on Reddit described it this way: "I thought my dark stools were just from eating spinach. By the time I got to the ER, my hemoglobin was 6.2 - half of normal. I almost didn’t make it."
What to Do Right Now If You Suspect an Overdose
If you see any of these signs, don’t wait. Don’t call your doctor tomorrow. Don’t check online. Call 911 or go to the nearest ER now.
While you wait for help:
- Do not take another dose - even if you think you missed one. More will only make it worse.
- Don’t take aspirin, ibuprofen, or naproxen - these make bleeding worse.
- Write down what you took - name of drug, dose, time taken. Bring the bottle if you can.
- Lie down - this helps slow blood flow and prevents fainting.
- Elevate bleeding areas - like a nosebleed or cut - above your heart if possible.
- Apply firm pressure to any external bleeding for at least 10 minutes without checking.
Don’t try to "wait it out" or take vitamin K at home. Vitamin K works - but only under medical supervision. Giving it yourself can delay critical treatment.

How Doctors Treat Blood Thinner Overdose
Emergency care depends on which drug you took and how bad the bleeding is.
For warfarin: If your INR is high but you’re not bleeding, doctors give oral vitamin K (1-5 mg). If you’re bleeding, they give 4-factor Prothrombin Complex Concentrate (PCC) - a concentrated clotting factor mix - along with IV vitamin K. PCC works in minutes. FFP (fresh frozen plasma) is used if PCC isn’t available, but it takes longer and can overload your heart.
For DOACs (Eliquis, Xarelto, Pradaxa): Specific antidotes exist. Idarucizumab (Praxbind) reverses Pradaxa in minutes. Andexanet alfa (Andexxa) reverses Eliquis and Xarelto. These cost $3,500-$10,000 per dose, but they work fast and save lives. Activated charcoal can help if taken within an hour of overdose, but it’s useless after that.
For massive overdoses - like someone taking 400 mg of warfarin - doctors may need to monitor INR for days. Effects can last up to 9 days. That’s why hospitalization is often needed, even if you feel okay at first.
Why People Delay - And Why That’s Deadly
A 2022 study found that 28% of people with warfarin-related bleeding waited more than 12 hours before seeking help. Why? They thought:
- "It’s just a nosebleed - I’ve had them before."
- "My stool is dark - must be the iron pill."
- "I’m tired because I didn’t sleep well."
- "I’ll wait until morning."
But every hour counts. The National Blood Clot Alliance found that people who got help within 2 hours of symptoms had a 97% survival rate. Those who waited 6+ hours? Only 76% survived.

How to Prevent an Overdose Before It Happens
Most overdoses are preventable. Here’s how:
- Know your INR target - most people need 2.0-3.0. If you have a mechanical heart valve, it’s 2.5-3.5. Ask your doctor to write it down.
- Get regular INR tests - weekly at first, then monthly if stable. Use a home monitor if your doctor recommends one - studies show they cut bleeding risk by 34%.
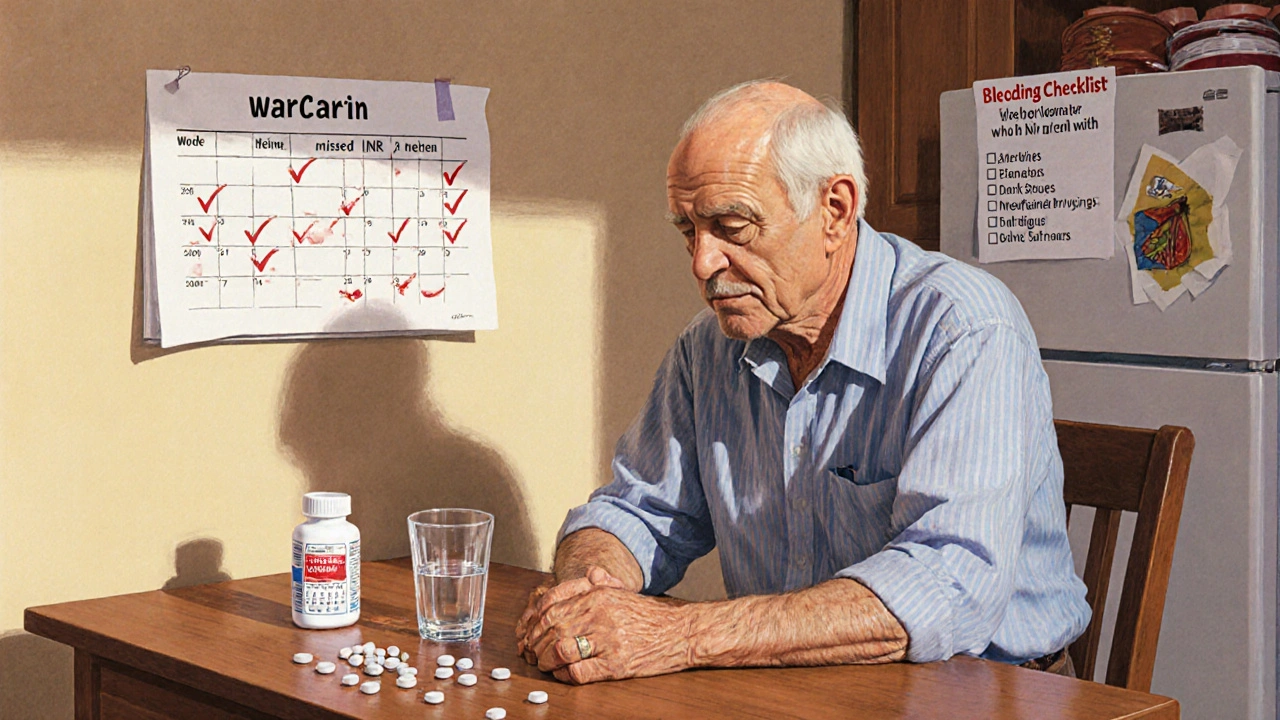
- Keep a bleeding checklist - print it and tape it to your fridge. Include: unusual bruising, bleeding gums, dark stools, red urine, headaches.
- Use a pill organizer - set alarms. Don’t rely on memory.
- Tell every doctor you see - even dentists. Many over-the-counter meds and supplements (like fish oil, ginkgo, garlic) increase bleeding risk.
- Avoid alcohol - it boosts warfarin’s effect and damages your liver, which makes INR harder to control.
- Know your reversal agents - if you take a DOAC, ask your doctor: "What’s the antidote? Where is it available?" Keep the name handy.
What Happens After an Overdose
Surviving an overdose doesn’t mean you’re safe. Many patients need to switch medications. Warfarin requires constant monitoring. DOACs are easier but cost more and need kidney checks. Some people can’t take either and need alternative treatments.
Follow-up care is critical. Your doctor will likely:
- Adjust your dose or switch drugs
- Check your liver and kidney function
- Review all your other meds
- Teach you how to recognize early bleeding signs again
One patient shared: "After my INR hit 9.1, they switched me from warfarin to Eliquis. I thought I’d be safer. But I still check my INR every two weeks - because now I know how fast this can kill you."
Can you reverse a blood thinner overdose at home?
No. While vitamin K helps reverse warfarin, it takes hours to work and must be given under medical supervision. Giving it yourself delays emergency treatment. For DOACs like Eliquis or Xarelto, there are no home reversal options. Only hospital-administered antidotes like idarucizumab or andexanet alfa work reliably. If you suspect an overdose, call 911 - don’t wait.
What happens if you take two blood thinners by accident?
Taking two different blood thinners together is extremely dangerous. Even if each dose is normal, they multiply each other’s effects. For example, taking warfarin and aspirin together can increase bleeding risk by up to 300%. If you accidentally take two, call poison control (1-800-222-1222) or go to the ER immediately. Do not wait for symptoms.
Do blood thinners cause bleeding every time you get a cut?
No. A small cut should still stop bleeding within 5-10 minutes with pressure. If you bleed longer than that - or bleed heavily from minor bumps - that’s a red flag. It’s not about every cut. It’s about unusual bleeding: slow stopping, large bruises, bleeding without injury. These are signs your blood isn’t clotting properly.
Can you survive a massive warfarin overdose?
Yes - but only with fast, aggressive treatment. One case involved a patient who took 450 mg of warfarin (over 100 times a normal dose). She survived because she reached the hospital within 3 hours. Doctors gave her PCC, IV vitamin K, and monitored her INR for 7 days. She had no permanent damage. But many don’t make it because they wait too long. Speed saves lives.
Is there a new reversal drug coming soon?
Yes. Ciraparantag is a new universal reversal agent currently in Phase III trials. It can reverse all types of anticoagulants - warfarin, DOACs, heparin - in under 10 minutes. If approved, it could replace PCC and antidotes, making overdose treatment faster and cheaper. But it’s not available yet. Don’t wait for it - use what works now.
Final Warning: This Isn’t a Risk You Can Gamble With
Blood thinners are life-saving - but they’re not safe unless you treat them like a loaded gun. One missed dose, one extra pill, one ignored bruise - it can end your life. The good news? You can prevent this. Know your numbers. Know your signs. Act fast. Your life depends on it.
Jenny Lee
November 18, 2025 AT 12:08Just saw my INR was 4.8 last week and didn’t think twice. This post scared me into calling my doctor today.
Kevin Jones
November 20, 2025 AT 08:59Warfarin’s mechanism is vitamin K antagonism-simple biochemistry. But the clinical implications? Nonlinear. INR >4.5 is a coagulopathic tipping point. PCC is the gold standard reversal agent. Time is tissue-literally.
Evan Brady
November 22, 2025 AT 04:00People think "blood thinner" means you bleed easier from paper cuts. Nah. It’s about silent internal hemorrhage. That one guy with INR 9.1? He survived because he didn’t wait for "proof." You don’t need proof-you need a 911 call.
Saket Sharma
November 22, 2025 AT 19:54DOACs are corporate poison disguised as convenience. They cost $10K per dose? Who profits? Pharma. Who pays? You. Warfarin’s cheaper, predictable, reversible. Stop being seduced by marketing.
Shravan Jain
November 24, 2025 AT 14:49the article is good but u forgot to mention that liver enzymes affect warfarin metabolism. also, most pts dont know their target inr. its sad. also, why no mention of cyp2c9 polymorphisms? lol.
Joshua Casella
November 25, 2025 AT 12:03If you’re on a blood thinner, you’re not just a patient-you’re a data point in a life-or-death feedback loop. Track your INR. Log your meds. Know your reversal agent. This isn’t optional. It’s bio-logical discipline.
Brandon Lowi
November 26, 2025 AT 05:06They want you to believe DOACs are "safer"-but who’s funding the trials? Who controls the guidelines? The same conglomerates that sold you opioids as "non-addictive." Wake up. Vitamin K is the original antidote. Not some $10K magic bullet.
Premanka Goswami
November 26, 2025 AT 12:20They don’t tell you that the FDA approved DOACs because they’re profitable-not because they’re better. The real danger? They’re testing these drugs on poor people in India and Africa. You think your INR is bad? Try getting PCC in rural Bihar.
mithun mohanta
November 27, 2025 AT 20:25Let’s be honest: most patients are clinically illiterate. You can’t expect someone who confuses "anticoagulant" with "antibiotic" to manage a drug with a 10-day half-life. This isn’t a medical issue-it’s a societal failure of education.
Alex Boozan
November 28, 2025 AT 00:36Every time you skip an INR test, you’re playing Russian roulette with your organs. The system doesn’t care. Your doctor’s overworked. Your insurance won’t cover home monitors. So who’s left? You. And your will to survive.
Richard Couron
November 28, 2025 AT 01:37They’re hiding the truth-blood thinners are a gateway to lifelong dependency. Once you’re on them, they never let you go. They’ll switch you to DOACs, then charge you $500/month. And if you bleed? They’ll say "it’s your fault for not monitoring." Bullshit.
Leilani O'Neill
November 28, 2025 AT 18:48Irish hospitals have protocols for DOAC reversal. You get idarucizumab within 15 minutes. In the US? You wait for PCC availability. This isn’t healthcare-it’s a lottery. And you’re the sucker buying the ticket.
Erica Lundy
November 30, 2025 AT 03:51It is worth noting that the physiological response to anticoagulant overdose is not merely a pharmacokinetic phenomenon, but a systemic collapse of hemostatic equilibrium. The body’s compensatory mechanisms-platelet activation, vasoconstriction, fibrinogen sequestration-are overwhelmed before clinical symptoms manifest. This is why early recognition is not merely prudent-it is ontologically imperative.
Alexis Paredes Gallego
November 30, 2025 AT 16:57Why do you think they don’t teach you this in med school? Because if patients knew how fragile their lives are on these drugs, they’d revolt. They’d demand home INR machines. They’d refuse to pay $10K for antidotes. So they keep you scared, confused, and obedient.
Ram tech
December 1, 2025 AT 15:29bro this post is lit but why no mention of herbal stuff? like turmeric and ginseng? they mess with warfarin too. also i think the guy who wrote this works for pfizer.