Bladder Muscle Spasms: What They Are and How to Manage Them
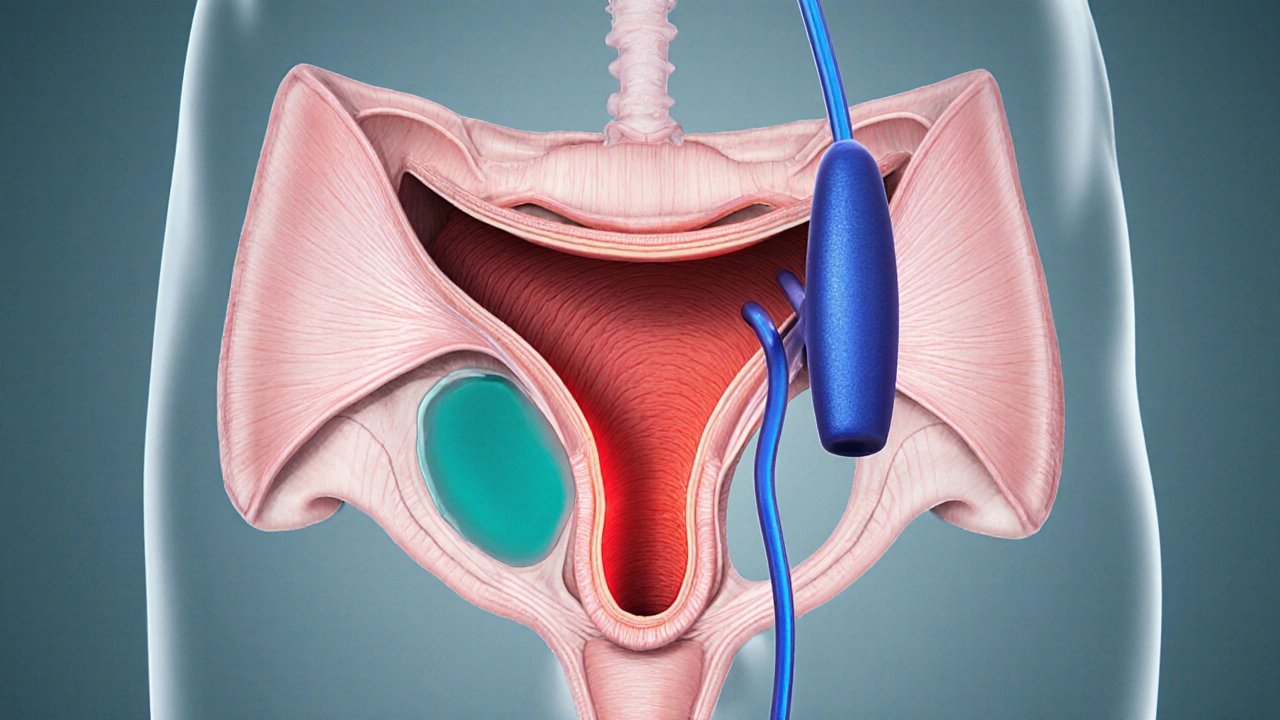
When dealing with bladder muscle spasms, involuntary contractions of the detrusor muscle that cause sudden urges to urinate, many people wonder why it happens. Also called detrusor overactivity, these spasms are a key sign of overactive bladder, a condition marked by frequent urgency, nighttime trips, and occasional leakage. They often show up alongside urinary urgency, the intense need to empty the bladder quickly and can be worsened by pelvic floor dysfunction, weak or uncoordinated pelvic muscles that fail to support proper bladder control. People with interstitial cystitis, a chronic bladder inflammation that causes pain and spasms also report similar episodes. Understanding these connections helps you choose the right strategy, whether it’s lifestyle tweaks, physical therapy, or medication.
So why do the muscles start twitching? The detrusor muscle, which lines the bladder wall, is normally controlled by a balanced nerve signal system. When that system goes haywire—often because of caffeine, alcohol, stress, or a urinary tract infection—the bladder receives “go” signals far too often. In jargon, we say bladder muscle spasms are triggered by hyperactive detrusor signaling. This hyper‑responsiveness is exactly what makes overactive bladder a chronic problem: the bladder thinks it’s full even when it isn’t. The result is a chain reaction—spasms create urgency, urgency drives frequent bathroom trips, and frequent trips can irritate the bladder lining, feeding back into more spasms. Think of it as a feedback loop where each entity influences the next.
Relief usually starts with breaking that loop. First, bladder training teaches the brain‑bladder connection to tolerate longer intervals between voids, directly targeting overactive bladder. Then, pelvic floor physical therapy strengthens the support muscles, reducing pelvic floor dysfunction and giving the bladder a more stable backdrop. If lifestyle tweaks aren’t enough, doctors may prescribe anticholinergic drugs or beta‑3 agonists, both of which calm the detrusor muscle. For those with interstitial cystitis, a diet low in acidic foods and bladder‑instilling therapies can lessen inflammation, which in turn lowers the frequency of spasms. In short, every treatment option addresses at least one of the related entities—whether it’s calming nerve signals, strengthening the pelvic floor, or soothing bladder inflammation.
Practical Steps to Keep Spasms in Check
Here’s a quick cheat‑sheet you can start using today: limit caffeine and alcohol to one serving each day; stay hydrated but avoid gulping large volumes at once; schedule bathroom breaks every 2‑3 hours to train your bladder; try Kegel exercises to reinforce pelvic floor strength; and keep a symptom diary so you can spot patterns and discuss them with your doctor. If you notice pain, cloudy urine, or a sudden increase in frequency, it’s wise to get checked for infection or interstitial cystitis. By tackling the root causes—overactive bladder, urinary urgency, pelvic floor dysfunction, or bladder inflammation—you’ll give yourself the best shot at easing those annoying muscle spasms.
Below you’ll find a curated list of articles that dive deeper into each of these topics, from the science behind detrusor overactivity to step‑by‑step guides on pelvic floor therapy and medication choices. Keep reading to discover the detailed information that can help you take control of your bladder health.
Urinary Retention & Bladder Muscle Spasms: What’s the Connection?
Discover why bladder muscle spasms often lead to urinary retention, how doctors diagnose the link, and what treatments-from meds to pelvic‑floor therapy-can restore normal flow.
view more