Opioid Safety: What You Need to Know
When working with opioid safety, the practice of reducing risks linked to opioid use while still managing pain effectively. Also known as opioid risk management, it guides clinicians, patients, and caregivers in safe prescribing, monitoring, and education. Understanding this field means looking at the whole picture: from how a drug works to what happens if it’s misused. That’s why opioid safety matters for anyone dealing with pain medication.
One core component is opioid addiction, a chronic condition where the brain adapts to the presence of opioids, leading to compulsive use. Addiction drives many of the safety concerns, so clinicians must screen patients, set clear expectations, and use the lowest effective dose. When addiction risk is high, alternative therapies become crucial.
Another vital tool is naloxone, an opioid antagonist that quickly reverses the effects of an overdose. Having naloxone on hand turns a potentially fatal event into a manageable emergency. Community programs now distribute kits to patients, families, and first responders, making overdose response faster and more effective.
Key Aspects of Opioid Safety
Effective pain management, the process of assessing and treating pain with a blend of pharmacologic and non‑pharmacologic methods relies on matching the right therapy to the right patient. For acute pain, short‑term opioids may be appropriate; for chronic pain, clinicians often combine lower‑dose opioids with physical therapy, cognitive‑behavioral strategies, or non‑opioid medications. This balanced approach reduces the chance of tolerance and dependence.
Guidelines also shape safe practice. The prescribing guidelines, evidence‑based recommendations that define dose limits, monitoring intervals, and documentation requirements set clear boundaries for clinicians. Following these rules helps catch early signs of misuse, such as escalating doses or missed appointments, and prompts timely interventions.
Patient education ties everything together. When patients understand how to take opioids, recognize side effects, and store medicines out of reach of others, they become active participants in safety. Simple steps—using a medication calendar, keeping a single pharmacy record, and knowing when to call a doctor—can prevent many problems before they start.
Monitoring tools add another layer of protection. Prescription Drug Monitoring Programs (PDMPs) let prescribers see a patient’s opioid history across the state, highlighting potential overprescribing or doctor shopping. Urine drug screens, when appropriate, verify that patients are adhering to the agreed plan and not mixing dangerous substances.
Finally, a safety culture means responding quickly when things go wrong. If a patient shows signs of overdose—extreme drowsiness, pinpoint pupils, or respiratory depression—administering naloxone and calling emergency services can save a life. Post‑event, clinicians should reassess the treatment plan, consider tapering, and connect the patient with addiction support services.
All these pieces—from addiction screening and naloxone availability to clear prescribing guidelines and robust patient education—form a network that makes opioid use as safe as possible. Below you’ll find a curated set of articles that dive deeper into each of these areas, offering practical tips, detailed comparisons, and the latest research to help you stay informed and protect those who rely on opioid therapy.
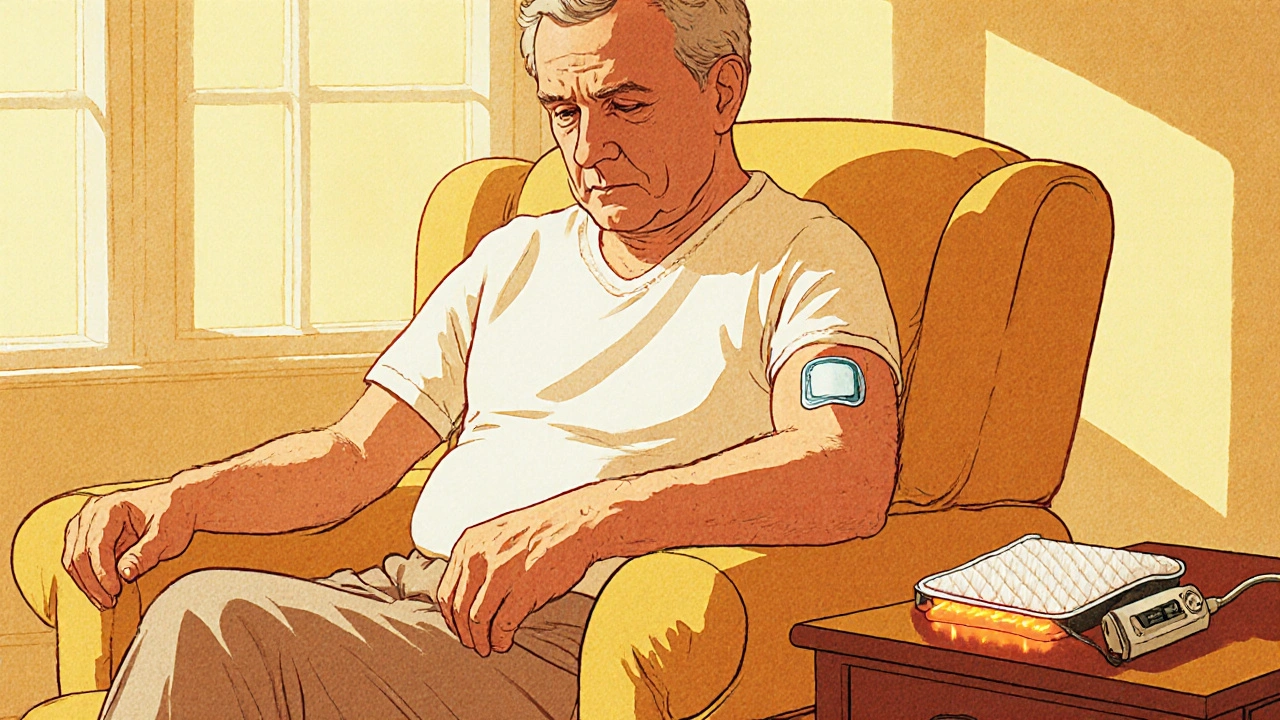
Heat Risks with Fentanyl Patches: How Heat Boosts Absorption and Increases Overdose Danger
Learn how heat boosts fentanyl patch absorption, the overdose risk it creates, and practical steps to stay safe. Real cases, science, and clear safety tips guide patients and caregivers.
view more