Overactive Bladder: What It Is and How to Manage It
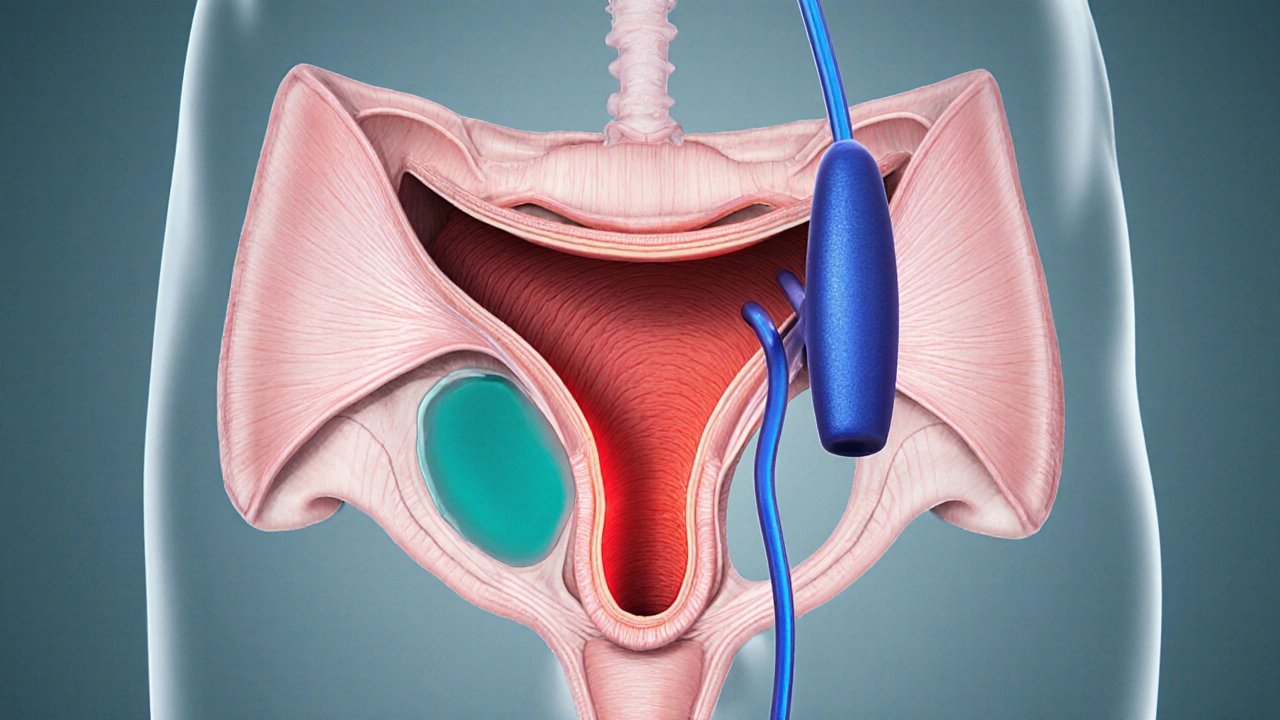
When dealing with Overactive Bladder, a condition marked by sudden urges to urinate, frequent trips to the bathroom, and occasional leakage. Also known as OAB, it affects millions and can disrupt daily life.
One of the core symptoms is Urinary urgency, the intense need to void quickly that can catch you off guard. This urgency often comes with increased frequency, especially at night, a problem called nocturia. If you notice yourself rushing to the nearest restroom multiple times a day, that’s a clear sign the bladder is overactive.
A proven strategy is Bladder training, a set of timed voiding exercises that gradually lengthen the interval between bathroom trips. The idea is simple: set a schedule, stick to it, and slowly push the limit. Over weeks, the bladder learns to hold more urine, reducing those frantic trips.
Medication options often involve Anticholinergic drugs, agents that relax the bladder muscle and lower involuntary contractions. These pills, such as oxybutynin or tolterodine, are a backbone of many treatment plans and can make a noticeable difference in urgency and leakage.
Another drug class gaining attention is Beta‑3 agonists, medications like mirabegron that relax the bladder without the dry‑mouth side effect of anticholinergics. They work by stimulating receptors that help the bladder store urine more comfortably, offering an alternative for people who can’t tolerate anticholinergics.
Physical therapy isn’t a side note—it’s a core part of the plan. Overactive Bladder can improve with regular pelvic floor exercises, known as Kegels, that strengthen the muscles supporting the bladder and urethra. Stronger muscles give you better control and reduce leakage episodes, especially when combined with bladder training.
Lifestyle tweaks also play a big role. Caffeine, alcohol, and carbonated drinks can irritate the bladder lining, making urgency worse. Cutting back on these triggers often leads to fewer sudden urges. Likewise, staying hydrated but spacing fluid intake throughout the day helps keep the bladder from getting overloaded at once.
Stress and anxiety can amplify symptoms, too. When you’re nervous, the body releases hormones that tighten the bladder muscle, mimicking an urgent need to go. Simple stress‑relief techniques—deep breathing, short walks, or mindfulness—can calm the bladder’s overreaction.
Putting all these pieces together creates a full picture: Overactive bladder encompasses urinary urgency, bladder training offers a behavioral fix, anticholinergic medication influences muscle activity, and pelvic floor strengthening supports control. By addressing the condition from several angles, most people find relief and regain confidence in daily activities.
Below you’ll find a curated list of articles that dive deeper into each of these topics—whether you want to understand the science behind urgency, compare medication options, or learn step‑by‑step training schedules. Browse the collection to get practical tips you can start using right away.
Urinary Retention & Bladder Muscle Spasms: What’s the Connection?
Discover why bladder muscle spasms often lead to urinary retention, how doctors diagnose the link, and what treatments-from meds to pelvic‑floor therapy-can restore normal flow.
view more