Pelvic Floor Dysfunction: What It Is and How It Affects You
When dealing with pelvic floor dysfunction, a condition where the muscles and connective tissue of the pelvic floor become weak or uncoordinated. Also known as pelvic floor disorder, it can impact bladder control, bowel movements, and sexual function.
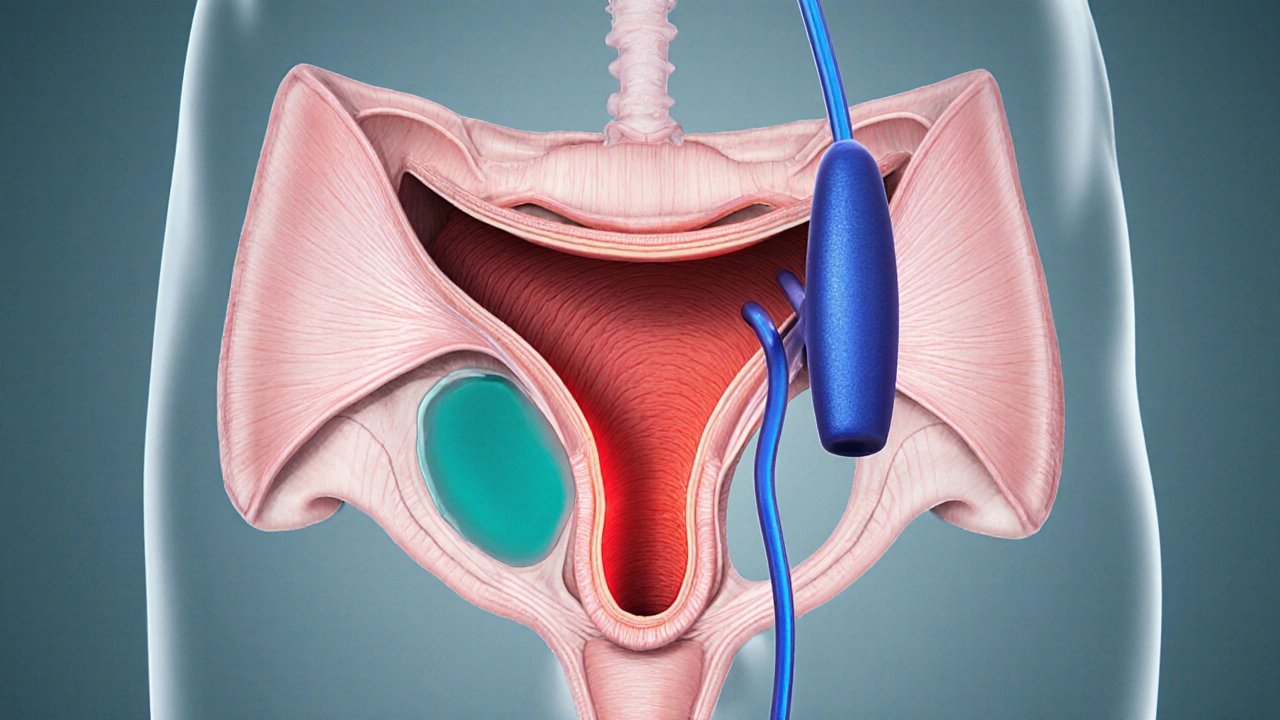
Understanding pelvic floor dysfunction is the first step toward relief. The pelvic floor is a sling of muscles that supports the bladder, uterus, and rectum. When that sling breaks down, a cascade of problems can follow. For many people, the most noticeable sign is urinary incontinence, where the bladder leaks during everyday activities.
Common Issues Linked to Pelvic Floor Dysfunction
Beyond incontinence, pelvic organ prolapse, the dropping of pelvic organs into the vaginal canal, often stems from the same muscle weakness. Chronic constipation can also be a symptom because the pelvic floor muscles struggle to coordinate proper bowel movements. These three conditions – urinary incontinence, prolapse, and constipation – form a triad that clinicians frequently see together.
Physical therapy offers a practical way to address the triad. Core strengthening exercises, especially targeted pelvic floor workouts, can rebuild muscle tone and restore coordination. Studies show that a regular regimen of Kegels, bridges, and diaphragmatic breathing reduces leak episodes by up to 40% in the first three months.
Pelvic floor dysfunction also influences sexual health. Weak muscles can lead to reduced sensation and difficulty achieving orgasm. By improving muscle control, many patients report better intimacy and confidence. This connection highlights why a holistic approach – combining exercises, lifestyle tweaks, and sometimes medical devices – works best.
When you start a treatment plan, assessment is key. A trained physiotherapist will evaluate pelvic floor strength, endurance, and coordination, then design a personalized program. This evaluation often includes EMG biofeedback, which lets you see muscle activity in real time and adjust technique instantly. The process underscores the principle that accurate measurement drives effective therapy.
In the articles below, you’ll find deep dives into how blood clots affect pelvic health, medication comparisons that matter for related conditions, and practical tips for everyday management. Whether you’re dealing with leakage, organ prolapse, or chronic constipation, the collection offers evidence‑based guidance to help you take control of your pelvic health.
Urinary Retention & Bladder Muscle Spasms: What’s the Connection?
Discover why bladder muscle spasms often lead to urinary retention, how doctors diagnose the link, and what treatments-from meds to pelvic‑floor therapy-can restore normal flow.
view more