Urinary Retention: Causes, Symptoms & Management
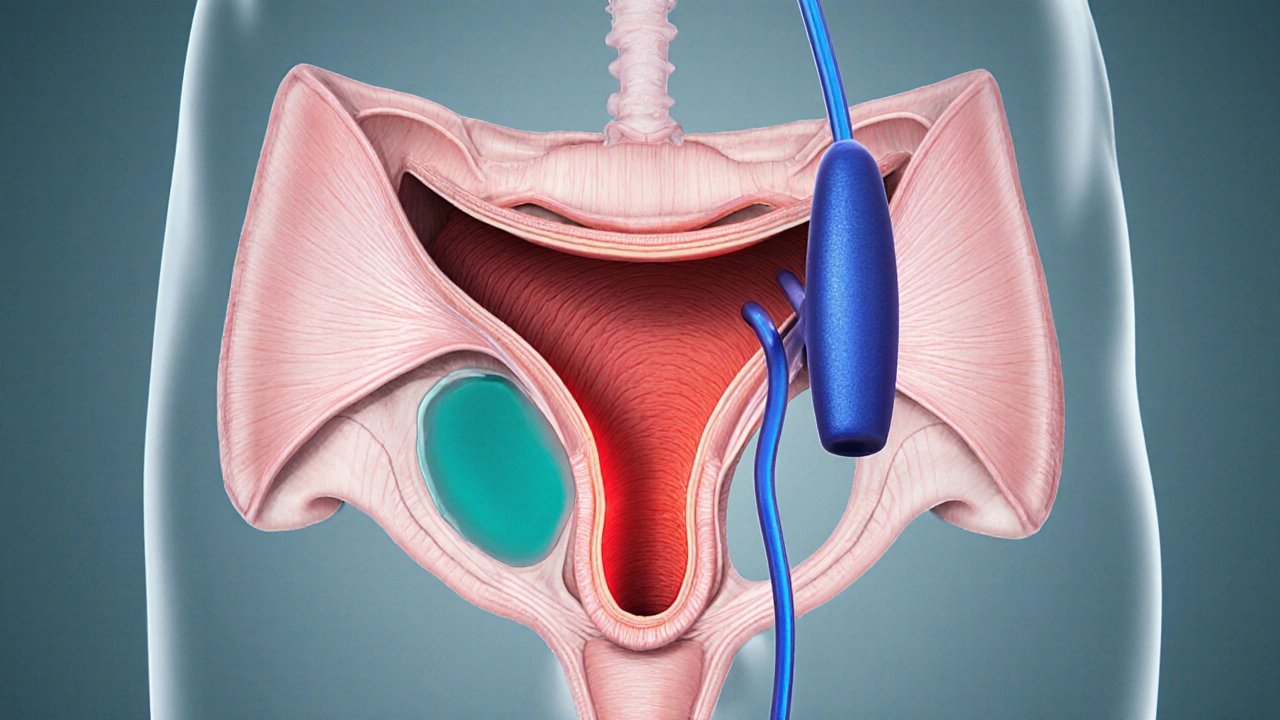
When dealing with urinary retention, the inability to fully empty the bladder, often causing discomfort and health risks. Also known as bladder retention, it can arise from many different sources. It often stems from problems in the bladder, the muscular organ that stores urine or from an enlarged prostate, a gland that can press on the urethra as it grows. Management may involve temporary catheterization, inserting a tube to drain urine safely. Understanding urinary retention helps you spot issues early.
Key Factors Behind Urinary Retention
One major driver is bladder dysfunction. When the detrusor muscle weakens or contracts erratically, the bladder can't push urine out efficiently. This dysfunction may be caused by neurological conditions such as multiple sclerosis, spinal cord injury, or diabetic neuropathy. Another common culprit is prostate enlargement. As the prostate grows, it narrows the urethral passage, creating resistance that the bladder must overcome. Men over 50 see a sharp rise in this issue, and the severity often correlates with gland size. Infections also play a part; a urinary tract infection can inflame the lining, making the flow sluggish and triggering retention episodes.
Because urinary retention encompasses these varied mechanisms, a thorough assessment is essential. Doctors usually start with a symptom checklist: difficulty starting urination, weak stream, a feeling of incomplete emptying, or sudden urge followed by little output. Physical exams may include a digital rectal exam to gauge prostate size, and a bladder ultrasound to measure post‑void residual volume. If the residual volume exceeds 150 ml, clinicians consider the condition significant. Lab tests can rule out infection, while urodynamic studies map pressure patterns inside the bladder and urethra, helping to pinpoint whether the problem is muscular, neural, or obstructive.
Treatment routes hinge on the underlying cause. For bladder muscle problems, pelvic floor therapy and medications like anticholinergics can improve coordination. Neurological contributors may respond to nerve‑stimulating devices or targeted rehab programs. When prostate enlargement is the primary factor, alpha‑blockers relax the prostate’s smooth muscle, and 5‑alpha‑reductase inhibitors shrink the gland over months. In more severe cases, minimally invasive procedures—such as transurethral resection of the prostate (TURP) or laser vaporization—create a wider passage for urine flow. If an infection triggers retention, a short course of antibiotics clears the inflammation, often restoring normal emptying.
In urgent situations, immediate catheterization is the safest way to relieve pressure and prevent kidney damage. Intermittent (straight) catheters are inserted only when needed, while indwelling (Foley) catheters stay in place for longer periods. Both carry infection risks, so proper sterile technique and timely removal are crucial. Some patients learn self‑catheterization, giving them independence and reducing hospital visits. For chronic cases, surgeons may recommend a suprapubic catheter placed directly into the bladder through the abdomen, bypassing the urethra entirely.
Beyond medical interventions, lifestyle tweaks can reduce the chances of retention returning. Staying hydrated, limiting caffeine and alcohol, and timing bathroom trips—so you don’t hold urine for too long—help keep the bladder working smoothly. Kegel exercises strengthen pelvic muscles, supporting better bladder control. Weight management also matters; excess abdominal pressure can worsen prostate symptoms and urinary flow. By understanding how bladder dysfunction, prostate growth, infections, and nerve issues intertwine, you can make smarter decisions about when to seek help and what treatments might work best. Below, you’ll find a curated set of articles that dig deeper into the science of clots, hypertension combos, immune‑related injury, food poisoning, Crohn’s disease, and more—each offering practical insights that tie back to the broader picture of urinary health and overall well‑being.
Urinary Retention & Bladder Muscle Spasms: What’s the Connection?
Discover why bladder muscle spasms often lead to urinary retention, how doctors diagnose the link, and what treatments-from meds to pelvic‑floor therapy-can restore normal flow.
view more