Every year, millions of pills, syringes, and inhalers go unused because they’ve passed their expiration date. In hospitals, nursing homes, and even home medicine cabinets, expired drugs sit unnoticed-until someone reaches for them in a hurry. The consequences can be serious: reduced effectiveness, dangerous side effects, or worse. But technology now makes it possible to stop this from happening-automatically, reliably, and at scale.
Why Manual Tracking Fails
For decades, checking expiration dates meant staff walking down aisles, scanning labels by hand, writing down dates on clipboards, and hoping nothing got missed. It’s slow, error-prone, and exhausting. A 2024 survey by the American Hospital Association found that 68% of pharmacies still had at least one expired medication in stock at any given time-despite regular checks. In emergency rooms, where speed matters, the risk is even higher. A nurse grabbing a vial from a crash cart doesn’t have time to read tiny print. And in home settings, families often forget to check until a bottle sits in the back of a cabinet for years.RFID: The Game-Changer for Hospitals
Radio Frequency Identification (RFID) is now the gold standard in hospital medication tracking. Each medication package is tagged with a tiny chip that holds its lot number, expiration date, and location. When a tray or cabinet is scanned, the system reads all items at once-up to 100 at a time-in under 30 seconds. Compare that to the 2-4 hours it used to take to manually count inventory. Systems like KitCheck is an RFID-based medication tracking platform that uses UHF tags to scan entire medication kits in seconds, with real-time expiration alerts and automated restocking are used in over 900 hospitals across the U.S. and UK. At Texas Children’s Hospital, pharmacists cut inventory time by 75% after switching to RFID. They also reduced expired drug waste by 18% in the first year. The system doesn’t just track expiration-it blocks access. If a medication is within two days of expiring, the cabinet won’t release it. No exceptions.eMAR: For Long-Term Care and Home Use
For nursing homes, home care agencies, and facilities serving people with intellectual disabilities, eVero is an electronic Medication Administration Record system that integrates with pharmacy systems to automate dosing schedules and send real-time alerts when medications are nearing expiration is the go-to solution. Unlike RFID, which tracks physical location, eMAR focuses on who took what, when, and whether it’s still safe to use. It syncs with pharmacy orders, so when a new prescription arrives, the system auto-enters the expiration date. Staff log doses via tablet or mobile app, and the system flags anything expiring in the next 72 hours. One UK-based care provider reported that before eMAR, they were throwing away 120 bottles of insulin per year because they expired before use. After implementation, that number dropped to 7. The system also helps with audits-regulators can pull up digital logs showing every dose administered, with timestamps and staff IDs.Automated Dispensing Cabinets (ADCs) and DrugXafe
Closed-door pharmacies and high-security units rely on Automated Dispensing Cabinets are intelligent storage units that automatically log medication details, lot numbers, and expiration dates when items are removed or restocked. These aren’t just locked boxes-they’re smart systems. When a nurse takes a painkiller, the cabinet records the exact time, patient, and drug. If the drug is expired, the door won’t open. The cabinet also alerts pharmacy staff when stock is low or nearing expiration. For supply chain tracking from manufacturer to bedside, DrugXafe is a pharmaceutical tracking platform that uses electronic product codes (EPCs) to monitor medications across the entire supply chain, automatically blocking sales of expired drugs uses unique barcodes tied to each pill batch. If a recall happens, the system instantly identifies every unit in every hospital, pharmacy, or clinic. It’s not just about expiration-it’s about safety at every step.
Mobile Solutions for EMS and Home Care
Emergency services don’t have the budget for full RFID setups. That’s where LogRx is a mobile app for EMS agencies that tracks controlled substances and expiration dates using existing smartphones, eliminating the need for new hardware comes in. Used by Portland Fire & Rescue and Elite EMS in the UK, LogRx runs on any iPhone or Android. Paramedics scan medication labels with their phone camera, and the app logs the expiration date. Alerts pop up if a drug expires in the next week. It’s simple, cheap, and integrates with DEA reporting tools. One UK EMS team said they went from spending 10 hours a week on paperwork to under 2. They also stopped getting fined for expired epinephrine auto-injectors-because now they replace them before they expire.What You Need to Get Started
Choosing the right system depends on your setting:- Hospitals with large inventories: Go for RFID systems like KitCheck. Expect to spend $50,000-$200,000 upfront, but save $120,000-$300,000 a year in reduced waste and labor.
- Long-term care homes: Use eMAR platforms like eVero. Integration with pharmacy systems is key-without it, data gaps create risks.
- EMS, clinics, home care: LogRx or similar mobile apps are ideal. No hardware needed. Just download, scan, and set alerts.
- Pharmacies managing controlled substances: ADCs with built-in expiration tracking are mandatory for DEA compliance.
- Assessment (2-4 weeks)
- Hardware/software setup (1-3 weeks)
- Staff training (2-6 weeks)
- Testing and go-live (2-4 weeks)
What’s Next? AI and Blockchain
The next wave is smarter automation. In early 2025, Intelliguard Health began piloting AI that predicts which drugs are likely to expire based on usage patterns. If a hospital rarely uses a certain antibiotic, the system suggests ordering less. It’s not just reacting to expiration-it’s preventing it. Blockchain is also being tested to track drugs from factory to patient. If a manufacturer tags a batch with a secure digital ledger, every pharmacy and hospital can verify its authenticity and expiration date without guesswork.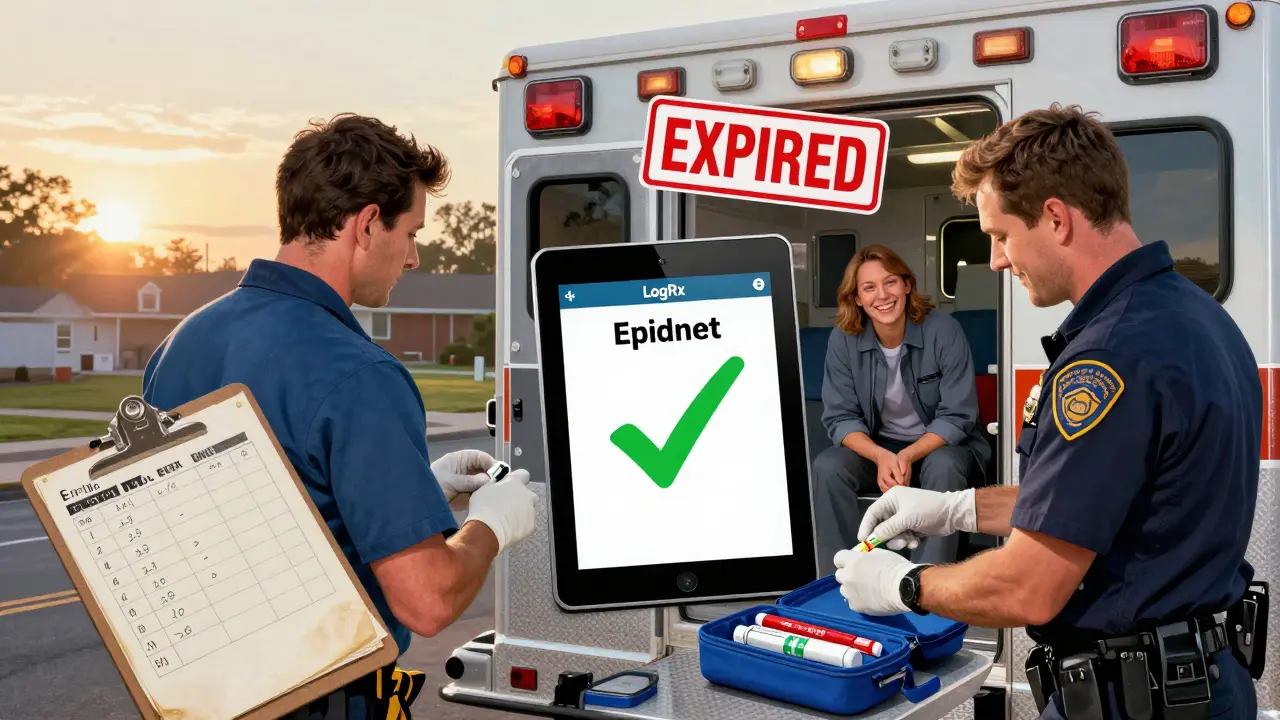
Real Results, Real Savings
The numbers don’t lie:- RFID systems reduce inventory time from hours to minutes
- Hospitals report 15-20% less expired medication waste
- EMS teams cut administrative work by 70%
- Compliance violations drop by over 90%
Final Thought: It’s Not Optional Anymore
Regulations from the FDA and DEA are tightening. By 2027, Gartner predicts 45% of U.S. hospitals will use RFID tracking. The UK is following closely. Waiting to act means risking patient safety, fines, and reputational damage. Technology isn’t here to replace staff-it’s here to free them from tedious, error-prone tasks so they can focus on what matters: caring for people.Can I use my phone to track medication expiration dates at home?
Yes. Apps like LogRx are designed for home care and EMS, but you can use any barcode-scanning app on your phone to scan medication labels and manually log expiration dates. Some apps, like Medisafe or MyTherapy, let you add pills and set reminders for when they expire. While not as automated as hospital systems, they’re far better than guessing.
Are expired medications dangerous to take?
Sometimes. Most medications lose potency over time, meaning they won’t work as well-like an antibiotic that doesn’t kill the infection. In rare cases, chemical breakdown can create harmful substances. Epinephrine in EpiPens, insulin, and nitroglycerin are especially risky if expired. When in doubt, don’t use it.
How much does RFID medication tracking cost?
Implementation costs range from $50,000 for small clinics to $200,000 for large hospitals. This includes tags, scanners, software, and training. But most facilities recover the cost within 12-18 months through reduced waste, fewer staff hours spent on inventory, and avoiding regulatory fines.
Do all medications come with RFID tags?
No. Currently, only medications sent to hospitals or large pharmacies are pre-tagged. Most retail drugs still use barcodes. Hospitals and systems like KitCheck add RFID tags themselves during inventory setup. Manufacturers are starting to adopt tagging, but it’s not yet universal.
What’s the difference between RFID and barcode tracking?
Barcodes require you to scan each item one at a time, line up the scanner, and manually enter lot numbers. RFID lets you scan entire trays or cabinets at once-even if items are stacked or covered. RFID reads faster, more accurately, and without human input. Barcode systems are cheaper but slower and more error-prone.
Can these systems work offline?
Some can. Mobile apps like LogRx store data locally on the phone and sync when Wi-Fi is available. RFID systems like KitCheck require network access for real-time alerts, but many cabinets have local backup modes that store expiration data and sync later. Always confirm offline capabilities with your vendor before purchasing.
Is this technology only for hospitals?
No. While hospitals lead adoption, the same tools are used in nursing homes, hospices, home care agencies, pharmacies, and even by paramedics. There are solutions for every scale-from a single ambulance to a 1,000-bed hospital.
Next Steps: What to Do Today
If you’re in a healthcare setting:- Ask your pharmacy or admin team if they’re using any expiration tracking system.
- If not, request a demo of KitCheck, eVero, or LogRx based on your facility size.
- Start small-pilot the system in one unit, like the ER or ICU, before rolling out hospital-wide.
- Download a medication tracker app and input all your prescriptions.
- Set monthly reminders to check your medicine cabinet.
- Dispose of expired drugs properly-don’t flush them. Many pharmacies offer take-back bins.

Cassie Widders
January 10, 2026 AT 21:59Been using Medisafe for my mom’s meds at home. Simple, no fuss. Gets the job done. Still better than staring at a cabinet full of bottles wondering which one’s from 2020.
Konika Choudhury
January 11, 2026 AT 02:41India needs this shit yesterday. Our hospitals are still using paper logs and hoping for the best. Why are we still in the 90s while the US is already using AI to predict expiration? Pathetic.
Darryl Perry
January 11, 2026 AT 21:35RFID implementation cost is grossly overstated. Most hospitals pay $120K for the software license alone. Tags are pennies. Training is the real cost center. And nobody talks about how many nurses just disable the alerts because they’re too noisy.
Alex Fortwengler
January 13, 2026 AT 20:47Let me guess. RFID tags are secretly tracking your every move. And those "expiration alerts"? They’re just a front for Big Pharma to make you buy new pills. You think they want you to save money? Nah. They want you hooked. The system blocks expired meds? Sure. Until they release the "new improved" version with a new expiration date. Same bottle. Different sticker.
Windie Wilson
January 14, 2026 AT 01:56So let me get this straight. We’ve got AI predicting which drugs will expire, blockchain verifying every pill’s origin, and cabinets that won’t open if the med’s expired… but we still can’t get a decent coffee machine in the ER? Priorities, people. Priorities.
Ben Kono
January 15, 2026 AT 17:41LogRx works great on my phone but the camera won’t scan the tiny barcodes on insulin pens. Had to type it in manually. Took 5 minutes. Felt like I was doing my taxes. Why does everything have to be so hard
Rinky Tandon
January 16, 2026 AT 22:13The entire premise of this post is a catastrophic misallocation of resources. We’re spending six figures on RFID chips and AI prediction models while millions of patients in developing nations still can’t access basic analgesics. This isn’t innovation-it’s techno-solutionism wrapped in a white coat. The real crisis isn’t expired meds-it’s the systemic refusal to distribute existing meds equitably. You want to save lives? Stop obsessing over barcodes and start fixing supply chains. Or better yet, stop making drugs so damn expensive in the first place. The expiration date isn’t the problem. The profit motive is.
And don’t even get me started on the marketing fluff around "DrugXafe" and "eVero"-those are just rebranded enterprise SaaS products with fancy acronyms. The real innovation is the fact that someone finally figured out how to monetize inventory management. Congratulations. You turned a basic logistical function into a $200K consulting package.
Meanwhile, the nurse who’s supposed to use this system is working 12-hour shifts, getting paid minimum wage, and told to "just scan the thing." No training. No support. Just a tablet with a 30% battery life and a pop-up that says "EXPIRED: DO NOT USE." And you wonder why compliance is low? It’s not because they’re lazy. It’s because the system was designed for a fantasy hospital that doesn’t exist.
And yes, I know this is the same system that’s supposed to prevent "dangerous side effects." But let’s be real-how many of those side effects are actually caused by expired meds versus misdiagnosis, understaffing, or polypharmacy? You’re solving a 5% problem with a 95% budget. That’s not efficiency. That’s performative tech.
Blockchain for drug tracking? Cute. But if the manufacturer doesn’t tag the batch at the source, it’s just a glorified spreadsheet. And if the pharmacy doesn’t scan it on receipt? It’s digital theater. We’re not building a better system-we’re building a better PowerPoint.
And don’t get me started on the "home use" apps. You think grandma in rural Ohio is downloading LogRx? She’s still using a sticky note on the fridge. The tech isn’t the barrier. The digital divide is. But nobody wants to talk about that because it’s not sexy. Nobody gets funding to train 70-year-olds to use a barcode scanner. But hey, we can fund a $2M RFID rollout in a hospital that already has 12 nurses on break.
So yes, the tech works. But it works for the people who already have power, money, and infrastructure. For everyone else? It’s just another reminder that healthcare isn’t a right. It’s a product. And you’re just selling the upgrade.
Daniel Pate
January 17, 2026 AT 20:11If we’re going to automate expiration tracking, shouldn’t we also ask why so many drugs expire at all? Why does the supply chain produce 30% more than needed? Why do we stockpile antibiotics that expire in 18 months when the infection they treat might not emerge for five years? The system fixes the symptom-not the disease. We’re treating expiration like a glitch in the code when it’s actually a symptom of a broken economic model. We incentivize overproduction because it’s cheaper to make too much than to build flexible, demand-driven manufacturing. We reward hospitals for hoarding because reimbursement is tied to inventory. And then we slap RFID tags on it and call it innovation. It’s not. It’s just automation with a moral veneer.
And what about the environmental cost? Every RFID tag, every scanner, every server running eVero has a carbon footprint. We’re replacing paper waste with electronic waste. Are we really sure this trade-off is worth it? The post says "it’s not just money-it’s lives." But what about the lives affected by the mining of rare earth metals for these chips? Or the e-waste dumped in Ghana because the system got upgraded after three years? We’re solving one ethical problem by creating another.
Maybe the real question isn’t how to track expiration-but how to design drugs that last longer. Or how to decentralize production so communities can make what they need, when they need it. Maybe the answer isn’t more tech-but less dependency on global supply chains. We’re so obsessed with fixing the symptom that we’ve forgotten to question the disease.