Theophylline-Ciprofloxacin Dose Calculator
Based on clinical guidelines, theophylline dose should be reduced by 30-50% when ciprofloxacin is prescribed. Most institutions use a 33% reduction as the standard adjustment.
Important: This calculator applies a 33% dose reduction based on ASHP guidelines. Always:
- Check baseline theophylline levels before starting ciprofloxacin
- Monitor levels every 24-48 hours
- Adjust further if levels exceed 20 mg/L
Recommended Dose Adjustment
For patients taking $0 mg/day of theophylline:
mg/day (33% reduction)
This adjustment aligns with ASHP guidelines to prevent toxicity when ciprofloxacin is prescribed. Remember to monitor levels closely and adjust further if needed.
When a clinician prescribes Ciprofloxacin a fluoroquinolone antibiotic that’s widely used for respiratory and urinary infections to a patient already taking Theophylline a methyl‑xanthine bronchodilator for COPD and asthma, the risk of serious toxicity can jump dramatically. This article walks you through why the interaction happens, who’s most vulnerable, and exactly what steps to take so the combo never turns dangerous.
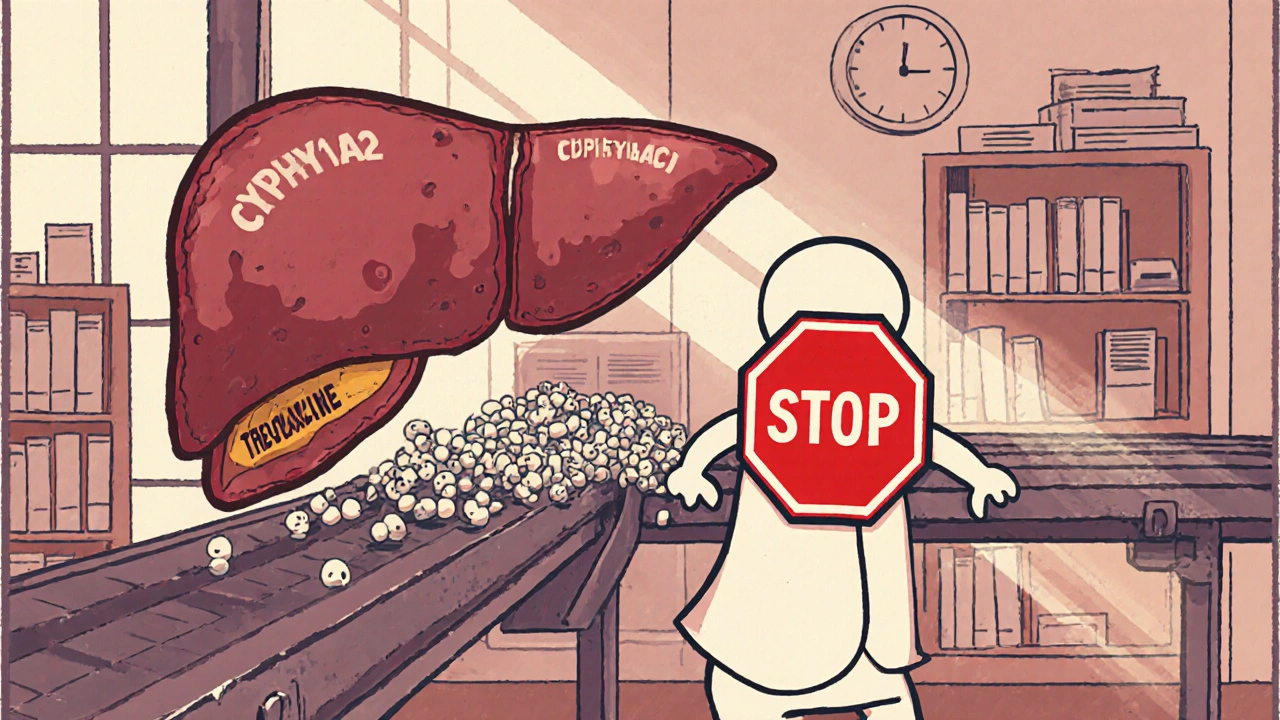
Why the Two Drugs Clash
Theophylline is cleared mainly by the liver enzyme cytochrome P450 1A2 (CYP1A2). Ciprofloxacin is a potent inhibitor of that same enzyme, cutting theophylline clearance by up to 45 % in older adults. The result? Theophylline’s area under the curve (AUC) swells by 40‑80 % and its half‑life stretches from the usual 8‑9 hours to 12‑15 hours. Because theophylline has a narrow therapeutic index of 10‑20 mg/L, even a modest rise can push concentrations into the toxic zone.
Clinical Evidence That Can’t Be Ignored
- First case report (Thomson et al., 1987) showed clearance dropping from 2.3 L/h to 0.8 L/h after ciprofloxacin was added.
- Population‑based nested case‑control study (Antoniou et al., 2011) found a 1.86‑fold higher odds of hospitalization for theophylline toxicity when ciprofloxacin was co‑prescribed.
- JAMA Internal Medicine (1990) described a 93‑year‑old patient who seized after just a few days of combined therapy.
- Meta‑analysis (Clinical Pharmacokinetics, 2015) calculated an average 45 % reduction in theophylline clearance for patients > 65 years.
Who’s at Highest Risk?
Age is the biggest driver-elderly patients often have reduced renal function and slower drug metabolism. Other risk amplifiers include:
- Pre‑existing high theophylline levels (≥ 15 mg/L).
- Genetic polymorphism CYP1A2*1F, which can deepen the inhibitory effect by ~65 %.
- Concurrent use of other CYP1A2 inhibitors (e.g., fluvoxamine, oral contraceptives).
- Severe infections that demand high‑dose ciprofloxacin (750 mg BID vs 500 mg BID).
Symptoms to Spot Early
Theophylline toxicity follows a dose‑dependent pattern:
- 20‑25 mg/L: Nausea, vomiting, headache.
- 25‑30 mg/L: Tachycardia, arrhythmias, hypertension.
- > 30 mg/L: Seizures, coma, possible death.
Because the interaction can raise levels within 24‑48 hours, clinicians should watch for any new neuro‑cardiac signs after starting ciprofloxacin.
Guideline‑Backed Management Steps
The American Society of Health‑System Pharmacists (ASHP, 2023) outlines a clear workflow:
- Obtain a baseline theophylline concentration before the first ciprofloxacin dose.
- Reduce theophylline dose by 30‑50 % (most institutions use a 33 % cut).
- Re‑check theophylline level every 24‑48 hours while both drugs are on board.
- If the level exceeds 20 mg/L, either hold theophylline or switch ciprofloxacin to a non‑interacting fluoroquinolone.
- Educate patients to report nausea, palpitations, or any seizure‑like activity immediately.
Choosing Safer Antibiotics
| Antibiotic | Effect on CYP1A2 | Increase in Theophylline AUC | Clinical Recommendation |
|---|---|---|---|
| Ciprofloxacin | Strong inhibitor | 40‑80 % | Avoid or reduce theophylline dose |
| Levofloxacin | Weak inhibitor | 10‑15 % | Usually safe; monitor if high‑risk |
| Moxifloxacin | Negligible | ~5 % | Preferred alternative when fluoroquinolone needed |
| Azithromycin | Minimal | ~2 % | Safe option for respiratory infections |
| Amoxicillin‑clavulanate | None | None | First‑line for many COPD exacerbations |
Practical Checklist for Clinicians
- ✔ Verify if the patient is on theophylline before writing ciprofloxacin.
- ✔ Review age > 65 years, renal function, and CYP1A2 genotype if available.
- ✔ Choose an alternative antibiotic (levofloxacin, azithromycin, amoxicillin‑clavulanate) whenever possible.
- ✔ If ciprofloxacin is unavoidable, cut theophylline dose by one‑third and schedule level checks.
- ✔ Document the interaction alert in the electronic health record; avoid overriding without justification.

What to Do If Toxicity Happens
Stop ciprofloxacin immediately. Supportive care depends on symptoms:
- Seizures - give benzodiazepines, consider activated charcoal if ingestion was recent.
- Arrhythmias - monitor ECG, correct electrolytes, and use anti‑arrhythmic agents as needed.
- Severe nausea/vomiting - anti‑emetics and IV fluids.
In extreme cases, hemoperfusion can remove theophylline, but this is rarely required.
Future Directions: Pharmacogenomics
Early‑phase trials at the University of Toronto (NCT04567890) are testing whether the CYP1A2*1F variant can predict who will need a larger dose reduction. Preliminary data suggest a 65 % greater drop in clearance for carriers. If validated, genotype‑guided dosing could become routine, especially for the growing elderly population.
Bottom Line
The ciprofloxacin‑theophylline interaction remains one of the most high‑severity drug‑drug combos in modern practice. By checking baseline levels, cutting theophylline dose, monitoring frequently, and opting for safer antibiotics, clinicians can almost entirely eliminate the risk of life‑threatening toxicity.
How much should I reduce theophylline when starting ciprofloxacin?
Guidelines usually recommend a 30‑50 % reduction, with many clinicians using a 33 % cut. Re‑check serum levels after 24‑48 hours and adjust further if needed.
Are all fluoroquinolones unsafe with theophylline?
No. Levofloxacin and moxifloxacin have minimal impact on CYP1A2 and increase theophylline exposure by only 10‑15 % or less, making them acceptable alternatives in most cases.
What are the earliest signs of theophylline toxicity?
Nausea, vomiting, and headache often appear once levels pass 20 mg/L. Tachycardia and arrhythmias follow at 25 mg/L, and seizures become a concern above 30 mg/L.
Should I order a CYP1A2 genetic test before prescribing ciprofloxacin?
Routine testing isn’t standard yet, but if the patient has a history of unexplained toxicity or is older than 80 years, a genetic screen can help tailor dose reductions.
What should I do if a patient on the combination develops a seizure?
Stop ciprofloxacin, give benzodiazepines, and consider activated charcoal if the ingestion was recent. Check theophylline level and arrange ICU monitoring for severe cases.
Monika Pardon
October 26, 2025 AT 13:42It is truly astonishing how quickly the pharmaceutical industry forgets its own warning labels, isn’t it? The ciprofloxacin–theophylline pairing appears to have been concocted by a boardroom eager to boost sales, regardless of the narrow therapeutic index. One could argue that the “guidelines” are merely a veil for profit‑driven research, especially when the interaction is so well‑documented. Nonetheless, clinicians who follow the checklist will at least protect a few vulnerable seniors from unnecessary harm.
Kasey Marshall
October 28, 2025 AT 21:15Ciprofloxacin inhibits CYP1A2 which is the main pathway for theophylline clearance. The result is a predictable rise in theophylline serum concentration. Older patients are especially at risk because their baseline clearance is already reduced. A 30 to 50 percent dose reduction of theophylline is a practical starting point. Baseline level measurement before starting the antibiotic helps set a reference. Rechecking the level after 24 to 48 hours catches any unexpected accumulation. If the level exceeds 20 mg per liter clinicians should consider holding theophylline. Switching to a fluoroquinolone with weaker CYP1A2 inhibition, such as levofloxacin, often avoids the issue. Azithromycin or amoxicillin‑clavulanate are other safe alternatives for respiratory infections. Patients should be educated to report nausea, palpitations or new headaches promptly. The interaction can develop within a day, so vigilance is essential during the early phase of therapy. Genetic testing for CYP1A2*1F is not routine but may guide dosing in high‑risk cases. In practice the checklist reduces hospitalizations for toxicity by a noticeable margin. Documentation in the electronic health record prevents accidental re‑prescribing. Ultimately the goal is to preserve the therapeutic benefit of both drugs without endangering the patient.
Jennyfer Collin
October 31, 2025 AT 04:49One cannot ignore the pattern of drug interactions that seem to slip through regulatory oversight, especially when a powerful antibiotic like ciprofloxacin is involved 😊. The data show a clear pharmacokinetic clash, yet the warning labels remain buried in fine print. Some may argue that the pharmaceutical lobby downplays these risks to keep market share alive. Nevertheless, the recommendation to reduce theophylline by a third is grounded in solid pharmacology. Clinicians who act on this guidance safeguard patients from a preventable iatrogenic crisis.
Laura Hibbard
November 2, 2025 AT 12:22Oh sure, because we all have endless time to recalcibrate doses mid‑shift, right? In reality, a quick dose cut and a level check is all it takes to keep the whole thing from blowing up. If you’re already juggling five patients, a short reminder in the chart does the trick. Let’s keep the momentum and make the safety steps part of the routine, not an after‑thought.
Rachel Zack
November 4, 2025 AT 19:55Doctors shoule always double check drug interactions before prescribing.
Lori Brown
November 7, 2025 AT 03:29Great summary! 👍 Following the checklist really does the trick, and patients feel much safer when we explain the signs of toxicity. Keep spreading the word, it makes a difference :)
Johnae Council
November 9, 2025 AT 11:02Honestly, the whole thing reads like a textbook exercise in risk management rather than real‑world practice. You get a list of steps, but where’s the discussion on workflow burden for busy wards? The recommendation to cut theophylline by a third is arbitrary without patient‑specific data. Also, the meta‑analysis you cite is over a decade old – newer agents might behave differently. I’d love to see a randomized trial comparing levofloxacin vs ciprofloxacin in this setting. Until then, we’re left to guess what works best.
Manoj Kumar
November 11, 2025 AT 18:35It is fascinating how we treat medicine like a game of chess, moving pieces without ever questioning why the board exists at all. Perhaps the real lesson is to accept uncertainty and focus on patient‑centered decisions rather than ticking boxes. If the guidelines feel like a bureaucratic maze, maybe it’s time to rewrite them with a dash of common sense. After all, the ultimate goal is to keep patients alive, not to satisfy an audit trail.
Hershel Lilly
November 14, 2025 AT 02:09The pharmacokinetic interaction described is straightforward: inhibition of CYP1A2 leads to elevated theophylline levels. From a clinical perspective, the most pragmatic approach is to anticipate the rise and adjust the dose proactively. Monitoring serum concentrations remains the gold standard for confirming safety. Incorporating these steps into the admission protocol can streamline care. This method balances efficacy of the antibiotic with the respiratory stability provided by theophylline.
Carla Smalls
November 16, 2025 AT 09:42Exactly, integrating the level check into the admission order set makes the process seamless for the team. A quick reminder note in the chart can prompt the nursing staff to draw the sample at the right interval. This small tweak can prevent a cascade of adverse events later on. Let’s keep sharing these practical tips so everyone benefits.
Rhea Lesandra
November 18, 2025 AT 17:15First, thank you all for the thorough discussion on this interaction. The core principle is simple: avoid letting theophylline levels climb into the toxic range. A concise way to remember is “check, cut, re‑check.” On the other hand, it is worth reflecting on how each step interlocks with broader patient safety initiatives, such as medication reconciliation, interdisciplinary communication, and continuous education of staff about high‑risk drug combinations. By embedding these actions into daily practice, we create a safety net that catches errors before they cause harm. Remember that even a brief pause to verify a dose can save a life. Let’s continue to champion these evidence‑based practices across all departments.
Dave Sykes
November 21, 2025 AT 00:49Spot on – the “check, cut, re‑check” mantra is exactly what we need on every shift. I’ve seen wards where this simple protocol reduced toxicity alerts by half. Let’s push for a standing order that automates the dose reduction when ciprofloxacin is prescribed. The data support it, and the patients deserve that level of protection.
Erin Leach
November 23, 2025 AT 08:22I appreciate how the article breaks down the warning signs; it helps us talk to patients in plain language. When you can point out that a new headache or jittery feeling might mean the drug levels are rising, it empowers them to call for help early.
Jay Campbell
November 25, 2025 AT 15:55Monitoring levels is essential.
Jacqui Bryant
November 27, 2025 AT 23:29Keeping the checklist handy makes the whole process easier for everyone involved.