Medication Sweating Relief Calculator
What medication are you taking?
Select your medication type to see evidence-based relief strategies.
More than 1 in 7 people taking prescription medications experience sweating or hot flashes as a side effect. It’s not just uncomfortable-it can make you quit your medicine. If you’re waking up soaked at night, drenched during a meeting, or avoiding social events because of sudden heat waves, you’re not alone. And you don’t have to just live with it.
Why Your Medication Is Making You Sweat
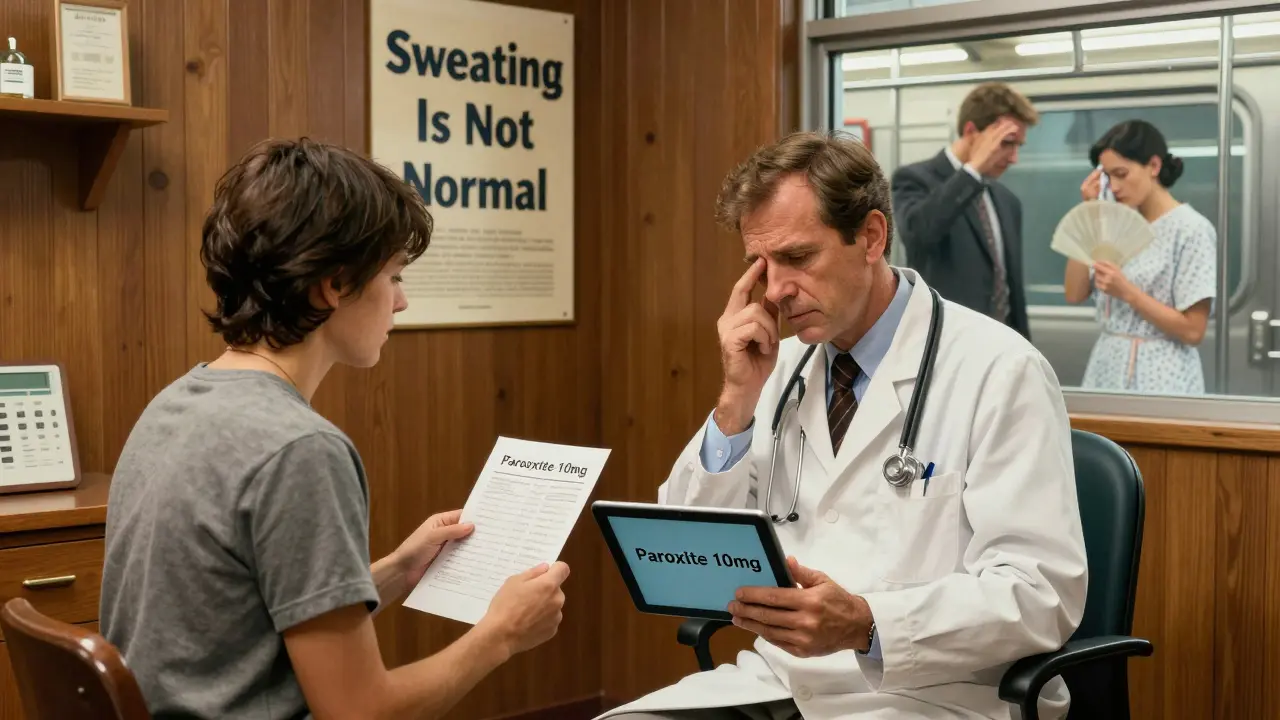
Sweating and hot flashes from drugs aren’t random. They happen because certain medications interfere with your body’s temperature control system. Your hypothalamus, the part of your brain that acts like a thermostat, gets mixed signals. Instead of keeping you at 98.6°F, it thinks you’re overheating-even when you’re not. Antidepressants are the most common culprits. Selective serotonin reuptake inhibitors (SSRIs) like sertraline (Zoloft) and escitalopram (Lexapro) cause excessive sweating in about 22% of users. The extra serotonin messes with how your body senses heat. SSRIs are also linked to night sweats, which affect over 30% of people taking them. ADHD stimulants like Adderall and Ritalin trigger sweating in nearly one-third of users. These drugs rev up your nervous system like a constant fight-or-flight response. Your heart races, your palms sweat, and your body tries to cool down-often too hard. Opioid painkillers such as oxycodone and morphine cause sweating in over 40% of users. This isn’t just from heat-it’s from histamine release. Your body reacts as if it’s under attack, even though the drug is meant to help. Hot flashes from cancer treatments are another major category. Drugs like tamoxifen and anastrozole block estrogen, which directly affects your body’s temperature control. Up to 78% of breast cancer patients on these drugs report daily hot flashes-some as bad as 20 times a day.How It’s Different from Normal Sweating
Primary hyperhidrosis-excessive sweating without a cause-is usually limited to specific areas: underarms, palms, or soles. Drug-induced sweating is different. It’s often generalized-you sweat all over. And it usually happens at night or right after taking your pill. It also shows up fast. If you started a new medication and two weeks later you’re drenched every morning, that’s a red flag. Stop and think: What changed? Most people don’t connect the dots until they’ve been struggling for months. The severity? It’s not mild for most. About 24% of people say their sweating is intolerable. And nearly 3 out of 10 stop taking their medication because of it. That’s dangerous. If you’re on blood pressure meds, antidepressants, or cancer drugs, quitting without talking to your doctor can hurt more than the sweating.What Actually Works to Reduce It
There’s no one-size-fits-all fix. But science-backed strategies do work.1. Prescription Antiperspirants
Over-the-counter antiperspirants often don’t cut it. The real solution? Aluminum chloride hexahydrate at 12-20%. Brands like Drysol or Xerac AC are prescription-strength and work by temporarily plugging sweat glands. Apply it to dry skin at bedtime-yes, even on your chest or back if you’re sweating there. Start with 2-3 nights a week. Most people see results in under 10 days. A 2023 study showed it reduces sweating by nearly 70% in drug-induced cases. It’s cheap, safe, and non-systemic-meaning it doesn’t affect your whole body.2. Timing Your Dose
If you take your pill at night, you’re more likely to sweat through your sheets. Moving your dose to the morning cuts night sweats by over half. This works especially well for antidepressants and ADHD meds. Talk to your doctor-some meds must be taken at night for other reasons. But for many, a simple switch makes a huge difference.3. Low-Dose Anticholinergics
For severe cases, doctors may prescribe glycopyrrolate at 0.5-1 mg daily. This blocks the nerve signals that trigger sweating. Clinical trials show it cuts sweat episodes by over 70%. Side effects? Dry mouth, blurry vision, constipation. But for many, it’s worth it.4. Non-Hormonal Options for Breast Cancer Patients
If you’re on tamoxifen or anastrozole and your hot flashes are unbearable, paroxetine (a low-dose antidepressant) is now recommended as first-line treatment. At just 10 mg daily, it reduces hot flashes by 62% without interfering with cancer therapy. It’s not a cure, but it’s a game-changer.5. Lifestyle Tweaks That Add Up
You don’t need expensive gear, but small changes help:- Wear moisture-wicking undershirts. They pull sweat away from your skin.
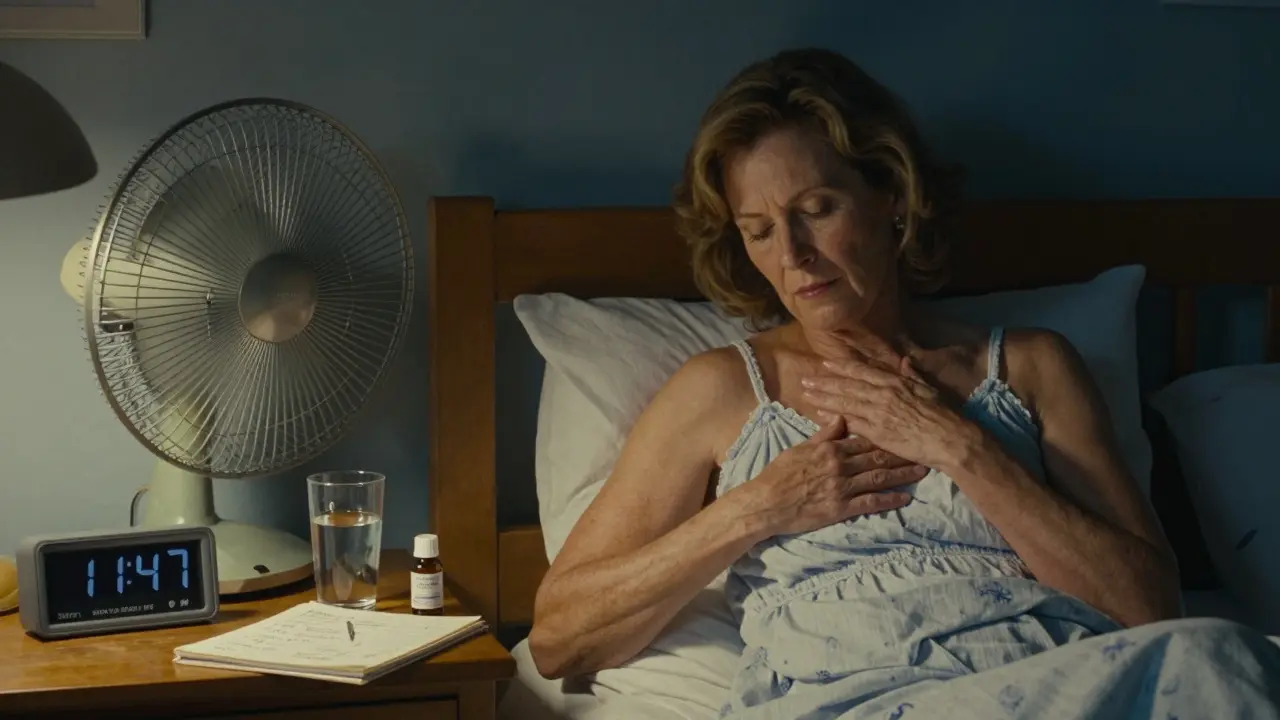
- Keep your bedroom under 65°F. Cooler temps reduce night sweats by 84%.
- Use layered clothing. Easily remove a layer when you feel a flush coming on.
- Avoid caffeine, alcohol, and spicy food. They trigger heat responses.
- Try cognitive behavioral therapy (CBT). Six to eight sessions can reduce hot flash severity by over half. It teaches you to manage the panic that often follows a flash.
What Doesn’t Work (And Why)
Many people try natural remedies-black cohosh, soy, acupuncture. Some report relief, but there’s no strong evidence they work for drug-induced sweating. Worse, some herbs interfere with cancer drugs or antidepressants. Don’t risk it. Surgery? Sweat gland removal or sympathectomy? These are rarely used now. Over 90% of people who get them end up with worse sweating elsewhere-called compensatory hyperhidrosis. Not worth it. And don’t assume your doctor will bring it up. A 2022 study found only 42% of primary care doctors routinely ask about sweating as a side effect. You have to speak up.When to Talk to Your Doctor
Don’t wait until you’re ready to quit your meds. If sweating is affecting your sleep, confidence, or daily life, schedule a chat. Bring this list:- Which meds you’re taking (include dosages)
- When the sweating started
- When it happens (day/night, after meals, during stress)
- How bad it is (mild, moderate, severe)
- What you’ve tried so far
- Switch you to a different drug in the same class
- Lower your dose slowly (25% reduction every few weeks)
- Add a non-hormonal treatment like paroxetine
- Refer you to a dermatologist or endocrinologist